Introduction
Radiation-based imaging has revolutionised the practice of modern medicine. Though it is used extensively in various fields of medicine, it remains the predominant modality for imaging in the cardiac catheterisation laboratory. However, these procedures place both the patient and the laboratory personnel at risk from ionising radiation. Excessive exposure to ionising radiation may have a deterministic effect from direct injury to skin or a stochastic effect in the form of neoplasms1. Professional societies have emphasised the need to develop radiation safety programmes for catheterisation laboratories, which include parties responsible for protection and safety, training/education of staff, radiation monitoring and protective shielding2,3. Guidelines have proposed a dose threshold of 5 Gy or 500 Gy·cm², beyond which patients must be monitored for skin injuries2.
In India, approximately 1,000 hospitals offer cardiovascular catheterisation facilities. The number of coronary interventional procedures increased from 177,240 in 2012 to 373,579 in 20164. An estimated 30% of these are multivessel or complex interventional procedures. In addition, approximately 30,000 non-coronary interventions are performed yearly and the number of diagnostic procedures is close to thrice the number of all other procedures performed4. Though there has been a steady growth in the number of catheterisation laboratories and procedures over the years, systematic reporting of patient radiation doses is not practiced in India. The aim of this study is to establish a baseline radiation reference dose for commonly performed coronary catheterisation procedures in India and to compare them with established international standards.
Methods
STUDY DESIGN AND POPULATION
This prospective observational study was conducted at four prominent tertiary cardiac centres across India. From June 2015 to January 2017, 4,603 consecutive patients undergoing diagnostic and interventional coronary procedures were prospectively included in the study. All the procedures were performed in accordance with the participating centres’ established internal standards. Procedures were categorised into the following three groups: Group I, coronary angiography (CAG); Group II, percutaneous coronary intervention (PCI); Group III, coronary angiography followed by ad hoc percutaneous coronary intervention (CAG+PCI). Other procedures such as peripheral, endovascular, structural, electrophysiological, or paediatric catheterisation were excluded. This study was approved by an ethical review board, and all patients signed an informed consent prior to the procedure. The study was registered with Clinical Trial Registry-India (CTRI), reference number: CTRI/2015/11/006359.
IMAGING EQUIPMENT
All procedures were performed using 3 Innova IGS 520 and 2 Innova 2100-IQ catheterisation laboratories (GE Healthcare, Chicago, IL, USA), installed between 2011 and 2015. All systems offered similar capability to customise dose and image quality among 5 “dose personalisation” settings according to the preference of individual institution. The choice of configurable settings, as well as the selection of acquisition frame rates and normal versus low dose level preference was left to the physician’s discretion. Together, configurable settings and selectable operational settings provided a typical 6:1 range in fluoroscopy and cine dose rate adjustment capability. The configurations of the system and selectable settings of acquisition protocols with radiation dose limit (RDL) used at the different hospitals are summarised in Supplementary Table 1. All systems provided built-in dosimetry capability, to monitor patient radiation data throughout the procedure.
DATA COLLECTION
The following data were prospectively collected for each procedure: baseline demographics, clinical characteristics of the patient, radiation dose indicators from the system at the end of the procedure (dose area product [DAP, Gy·cm²]) and cumulative air kerma [CAK, mGy], fluoroscopy time [FT, minutes]), as well as other procedural data such as procedure type, access route, number of vessels treated, number of stents implanted, duration of the procedure, procedural complications, quantity of contrast, use of adjunctive technology such as intravascular imaging, fractional flow reserve assessment and rotational atherectomy. In addition to the patient radiation data, other parameters such as acquisition mode, frame rate, radiation exposure data split between fluoroscopy and cine x-ray acquisition duration, and number of cine exposures were automatically recorded for each x-ray acquisition and were analysed. For comparison between institutions, DAP rates were used to normalise differences in procedural time, which might be attributed to differences in operator experience or complexity of the procedure5. For each type of procedure, radiation data reference levels (RLs) were established as the third quartile of the total distribution6. For this study, the 75th percentile of the distribution of DAP values was defined as dose reference level (DRL).
STATISTICAL ANALYSIS
Statistical analysis was performed using Microsoft® Excel® 2010 (Version 14.0.7165.5000) and Minitab® 17 statistical software (2010) (Version 17.3.1; Minitab, State College, PA, USA). Categorical variables are presented as numbers and percentages. Continuous variables are described with mean ± standard deviation or median (with interquartile range) depending on their distribution. Kruskal-Wallis test was used for one-way analysis of variance for comparison of radiation data between sites. Comparison of radiation data was performed using the one-sided non-parametric one sample sign test, when referenced data were provided as median, to test the null hypothesis that no difference would be found between study and reference median and with the alternative hypothesis that the study median would be lower than the reference median. Similarly, when referenced data was provided as mean, a one sample t-test was used. Multivariate analysis was performed for the patient subset of coronary interventions (PCI and CAG+PCI) to identify individual risk factors with logarithm-transformed DAP as the dependent variable using back-ward stepwise analysis. All the patient-related and image acquisition-related characteristics listed above were used as covariates. Beta-coefficients are given after re-transformation (exp [beta coefficient]) to describe the relative influence of each variable on DAP. A 95% confidence level was used for all statistical calculations and a p-value of 0.05 or less was considered significant.
Results
Overall 4,603 patients were included in the study. Of these 4,371 had analysable data (195 incomplete radiation datasets, and 37 excluded from analysis as other types of procedures). Procedure distribution, demographic profile, cardiovascular risk factors and indications for the procedure are summarised in Table 1. The majority of patients were male (71%). Diabetes and hypertension were prevalent at 39% and 42%, respectively. Most of the procedures were performed electively (69%). The impact of BMI on radiation is depicted in Figure 1, and there is a stepwise increase in DAPs in both PCI and CAG+PCI groups across increasing BMIs. This trend, however, is not seen in the CAG group. Procedural data are shown in Table 2. The transradial technique was used in 76% of the patients. There were 2,906 CAGs, 750 PCIs and 715 CAG+PCIs. Adjunctive technologies were used in 99 (2.9%) patients. On an average, there were 1.2±0.4 vessels treated and 1.3±0.6 stents implanted per each therapeutic procedure.
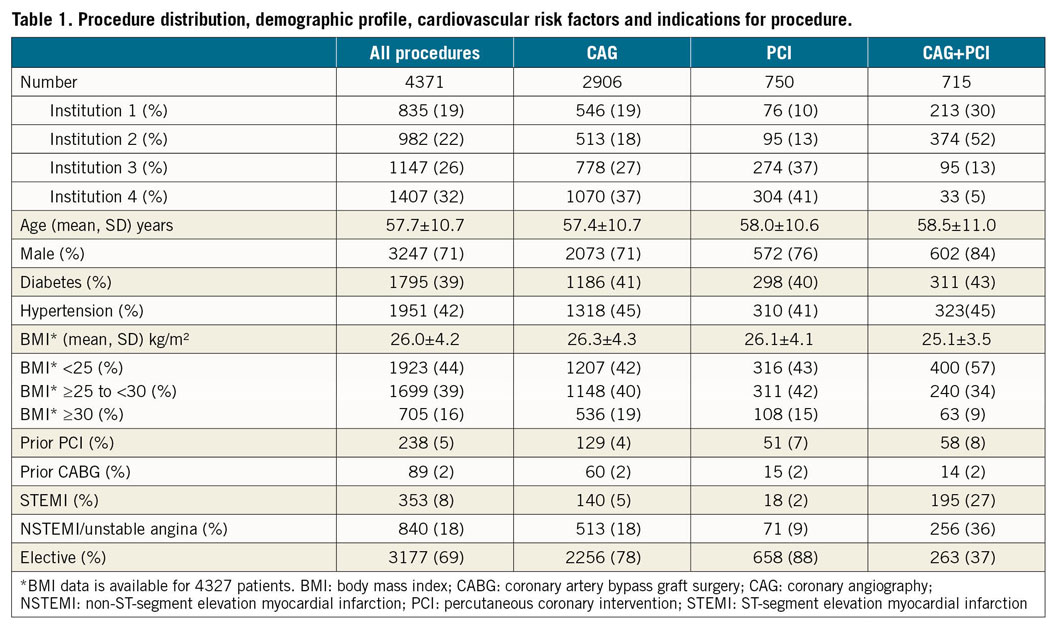
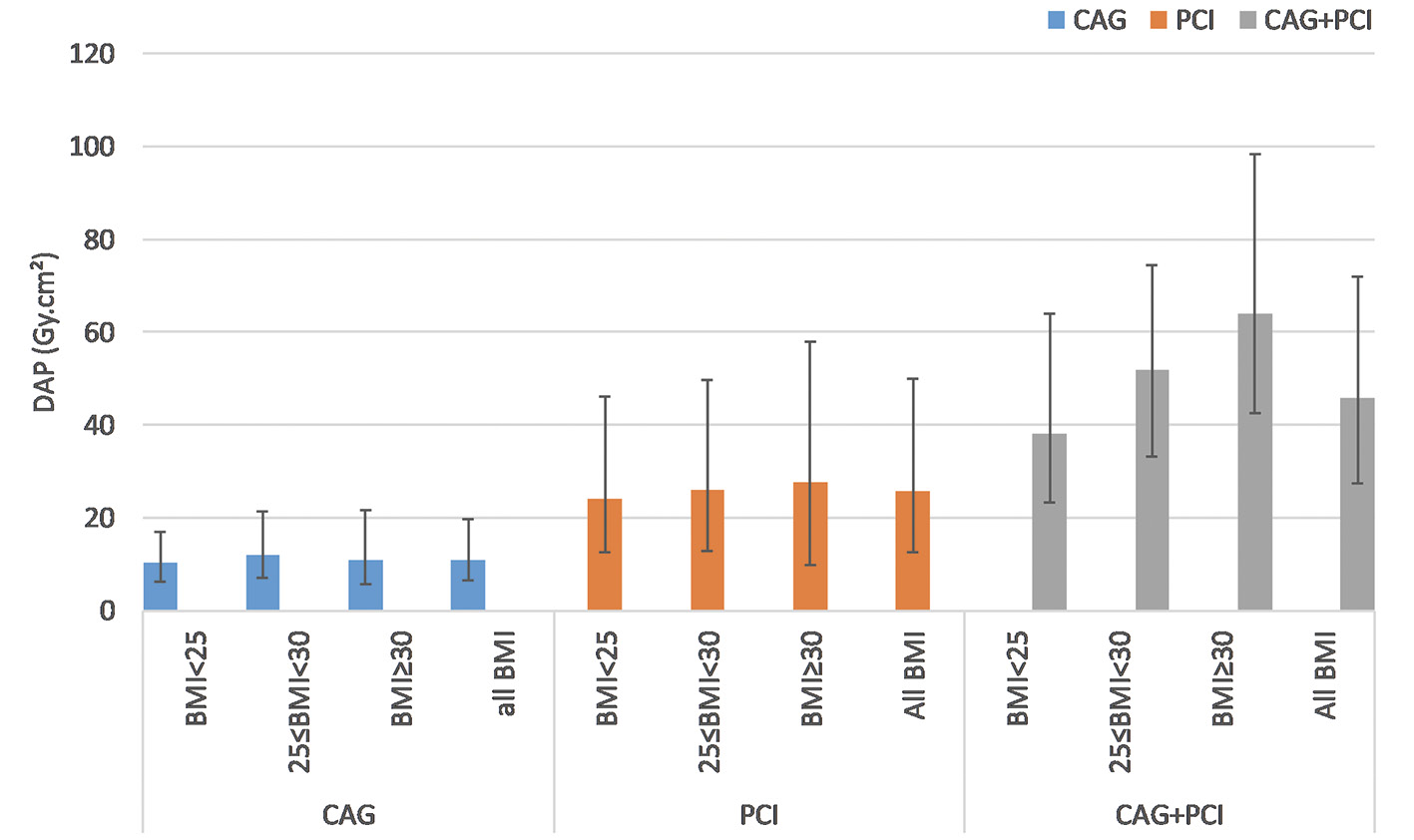
Figure 1. Impact of BMI on patient radiation dose. BMI: body mass index, DAP: dose area product
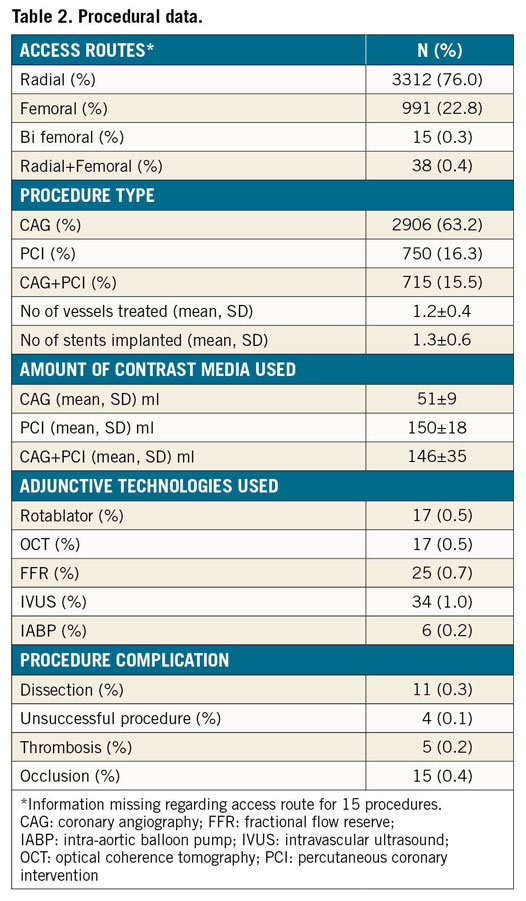
Procedure specific radiation data are summarised in Table 3. Reference levels for DAP, CAK and FT from the study for the above procedures were: 19.6 Gy·cm2, 325 mGy, 4.5 min for CAG; 49.8 Gy·cm2, 1016 mGy, 18.2 min for PCI; and 72.0 Gy·cm2, 1461 mGy, 15.1 min for CAG+PCI, respectively. As expected, both DAP level, CAK level, and number of cine frame rates were higher when ad hoc PCI was performed. Male gender, higher BMI, combining CAG+PCI, fluoroscopy time, number of cine frames, and image acquisition settings were significant contributors to increased radiation dose (Table 4). Among the fluoroscopy settings, using ‘7.5 fps RDL+Low’ significantly decreased DAPs while ‘15 fps Smart IQ Low’ did not show any statistical significance. On the other hand, 15 fps with either ‘Normal or Smart IQ Normal’ adversely impacted the DAPs. Similarly, cine settings at 15fps when used with ‘RDL+Low’ notably reduced the radiation levels while other cine settings did not. There was significant dispersion of 75th percentile of DAP between the 4 centres for all procedures (‘p’<0.05) (Figure 2). The maximal range of median DAP between centres was 7-21 Gy·cm²,13-52 Gy·cm², and 20-57 Gy·cm² for CAG, PCI and CAG+PCI respectively. Institution 4 had the lowest DAP median for each of the 3 groups and this was the only institution which used “7.5 frame/s RDL+Low” settings for fluoroscopy.
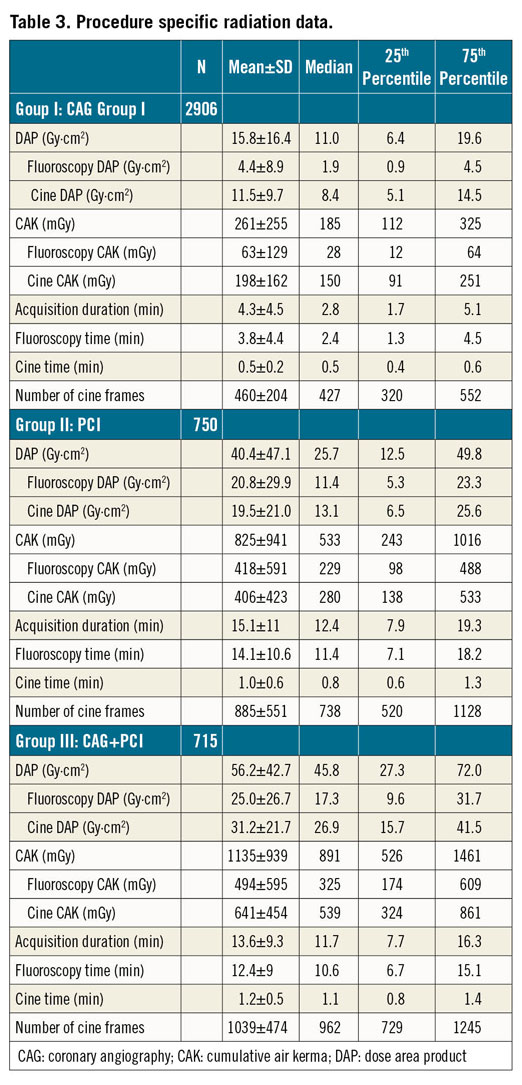
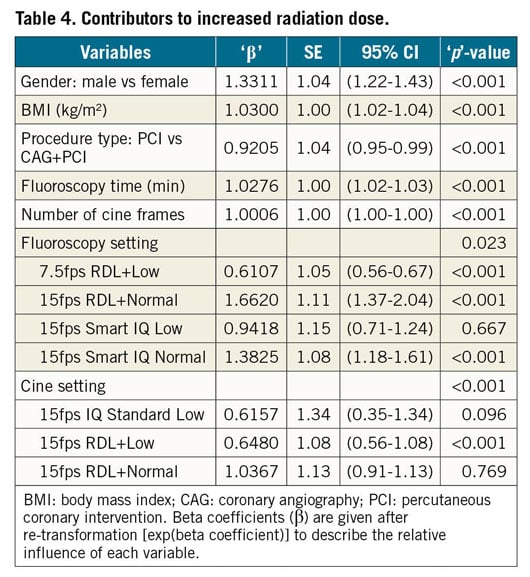
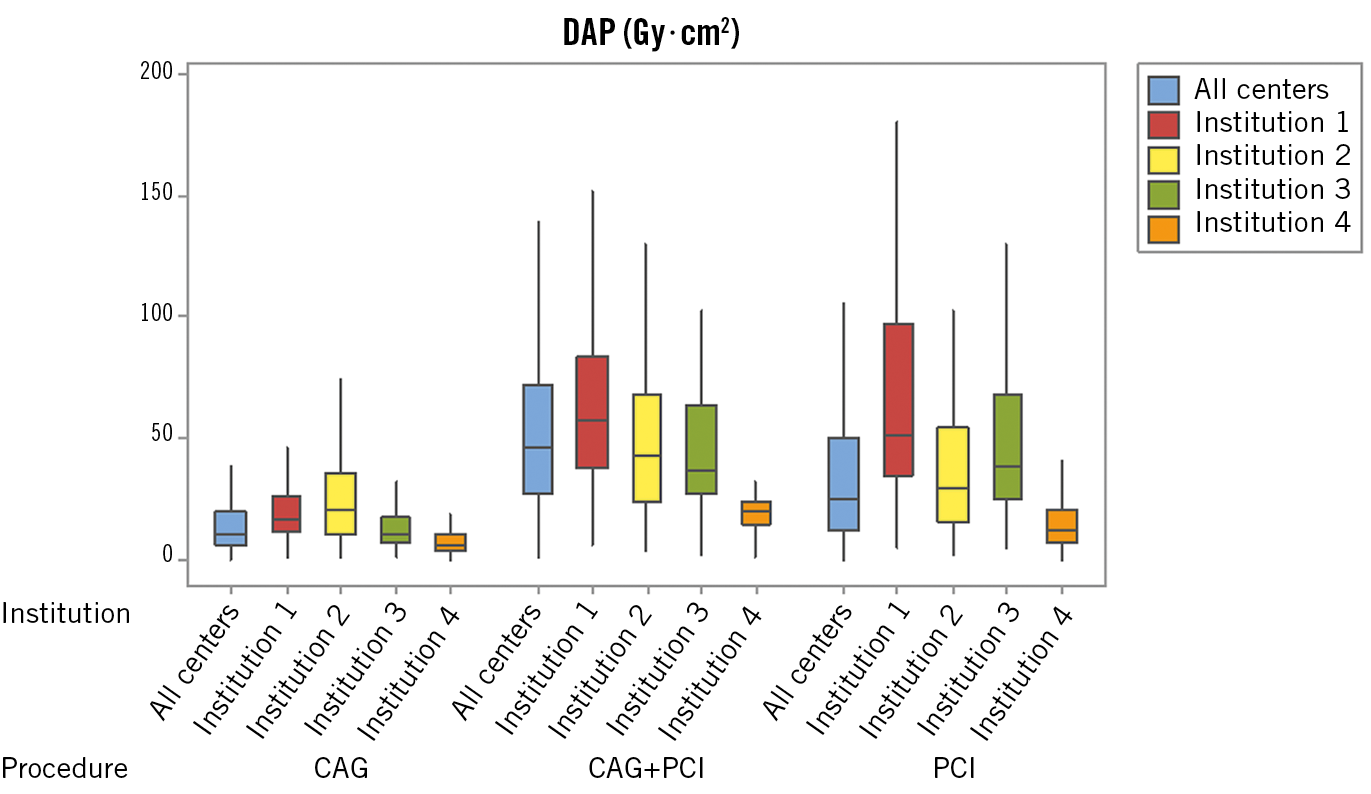
Figure 2. 75th percentile DAP data by institutions. CAG: coronary angiography; CAG+PCI: coronary angiography followed by percutaneous coronary intervention; DAP: dose area product; PCI: percutaneous coronary intervention
Distribution of CAK is depicted in Figure 3. Overall, 87.4% of the procedures were below 1 Gy, including 98% of CAG, 74% of PCI and 57% of CAG+PCI. 98.8% of the procedures were below the first notification threshold of 3 Gy. 1% of the examinations attained a radiation dose between 3 and 5 Gy. Only 0.3% of all PCIs (6 elective and 6 ad hoc) exceeded the substantial radiation dose level of 5 Gy, above which patient follow-up is recommended2. This category was inclusive of 3 patients with complex primary PCI, 4 PCIs for calcified lesions, 1 complex bifurcation PCI, 3 PCIs for chronic total occlusion, and 1 patient who had PCI-related complications. However, lesion complexity data was not included in the study analysis as it was not available for all patients. Comparison of radiation data from the current study with international references and recent literature are shown in Figure 4 as well as in Supplementary Table 2 and Supplementary Table 3,6,7,8,9,10,11,12,13,14,15,16. For each procedure category, the study median DAP and 75th percentile DAP were compared with data from previously published studies: 4 study datasets out of 31 had comparable or lower DAP for CAG and 9 out of 40 had similar outcomes for PCI. This trend also continued with comparisons of CAK and FT.
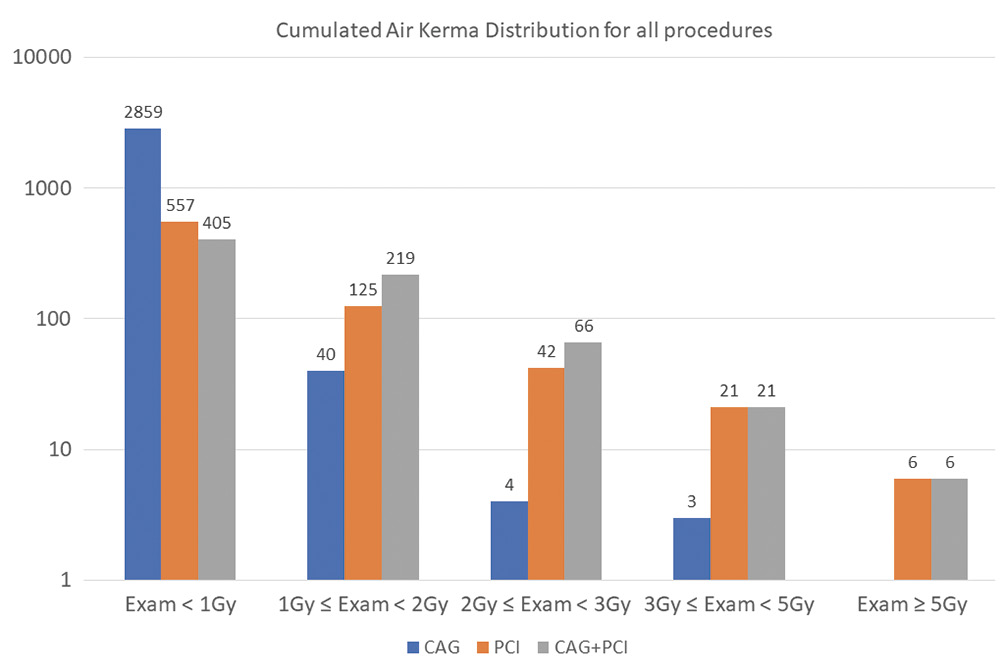
Figure 3. Cumulative air kerma distribution for all procedures, (CAG, PCI, CAG+PCI) – Log scale. CAG: coronary angiography; CAG+PCI: coronary angiography followed by percutaneous coronary intervention; PCI: percutaneous coronary intervention
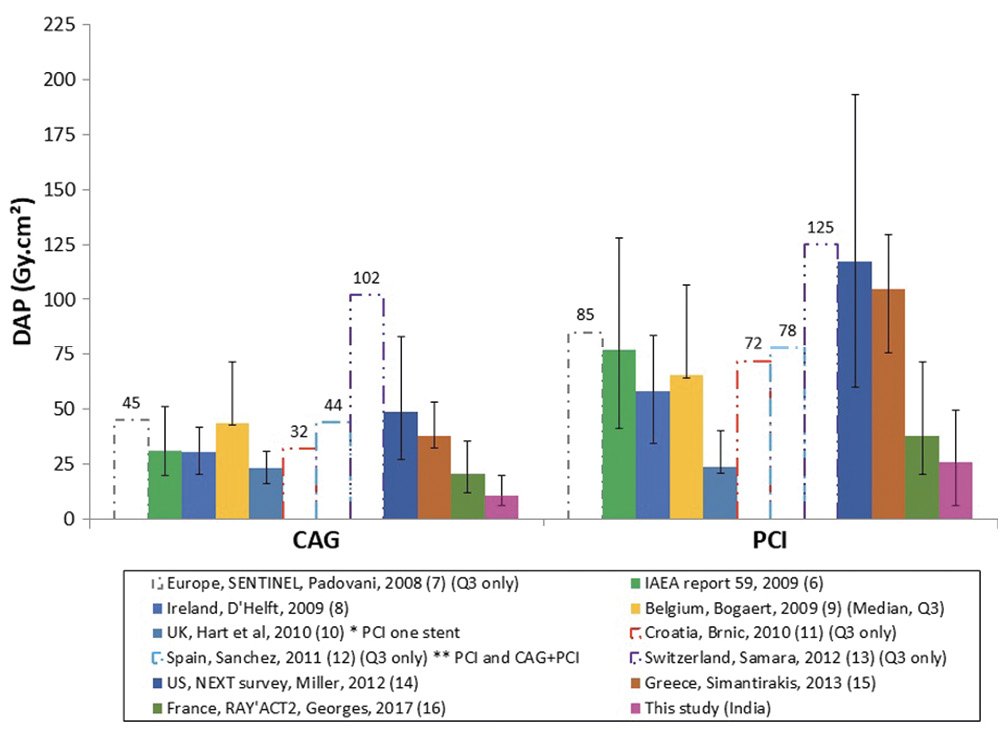
Figure 4. Cumulative DAP (Gy.cm²) in comparison with international references for CAG and PCI categories. Median and interquartile range are given, unless otherwise indicated. CAG: coronary angiography; DAP: dose area product; PCI: percutaneous coronary intervention
Discussion
The major observations of our study are firstly that DAP and CAK during diagnostic and interventional coronary procedures from a selection of Indian centres are comparable, and in the low range in reference to international standards. Secondly, only 1% of all the procedures received a dose between 3 Gy and 5 Gy and 0.3% of the examinations attained a dose above the cut-off value 5 Gy. Thirdly, there is considerable variation across the sites with regard to the radiation parameters. Fourthly, male gender, higher BMI, combining CAG+PCI, fluoroscopy time, number of cine frames, and image acquisition settings were significant predictors of higher DAP.
Historically, radiation dose during catheterisation procedures varies widely based on age, BMI, radial route, previous bypass grafting, lesion complexity, equipment generation, technical settings and operator experience17,18. Gender-based patterns for radiation exposure across catheterisation laboratories are unknown. In this study, male gender is an important predictor but women were under-represented (29%) and the significance of this finding after adjustment for lesion complexity is not analysed. However, in a study exploring mean effective radiation dose for nuclear cardiology procedures, it was shown that women required a slightly lower radiation dose (9.6±4.5 mSv) than men (10.3±4.5mSv, p<0.001)19. On the other hand, the adverse relationship between BMI and radiation dose is well established18. Ad hoc PCI increased DRL significantly, with mean DAP 56.2±42.7 Gy·cm2 where as the PCI group had a mean of 40.4±47.1 Gy·cm2. In a study published by Truffa et al20, the ad hoc group had lower total DAP 119.7±70.7 Gy·cm2, compared to the staged group, 139.2±5.3 Gy·cm2 (p<0.001), but the staged group’s total DAP included the radiation during both CAG and PCI, and thus cannot be compared to the present study. Fluoroscopy time, number of cine frames, and image acquisition settings are conventional risk factors of radiation18.
All the hospitals participating in the study have used the same equipment for X-ray imaging but the choice of configurable settings was left to the physician’s preference. At the institution which recorded the lowest mean DAP for all procedures, the physicians opted for low frame rates as well as low radiation protocols for all the procedures. Preference of image technical settings between sites to accomplish a clinical task, operator’s practice and awareness of radiation reduction techniques (such as usage of collimation while limiting magnification, limitation of steep angulations, optimal placement of image receptor as close as possible to the patient, selection of lower frame rates and lower dose level preference, use of fluoro-store function instead of cine) all have an impact on the levels of radiation. Georges et al17, in their analysis of 34,436 CAGs and 28,932 PCIs across 44 centres in France, observed significant differences in the radiation doses between participating centres. The maximal range of median KAP between centres was 9-54 Gy·cm² and 16-126 Gy·cm² for CAG and PCI respectively. When comparison was made between centres delivering lower and higher radiation doses, use of old equipment, routine left ventriculography, and use of frame rates >7.5 fps were more frequent in centres delivering higher doses.
The incidence of high dose exposure varies between 0.1% and 1.0% among different studies17. Historically, high radiation doses commonly occur in patients with high BMI and in those undergoing complex interventional procedures such as chronic total occlusions or treatment of calcified lesions or anomalous coronary arteries, or when procedure complications occur21. Similar findings were observed in this study and are consistent with other published studies17. None of the patients with radiation doses above 5 Gy reported skin injuries. However, the current study did not mandate follow-up of patients who received high radiation doses.
The main objective of any radiation dose assessment is to minimise the detrimental effects of radiation by reducing exposure to it in the catheterisation laboratory. DRLs serve as a benchmark that gives an opportunity for the individual laboratories to compare their performance and to adapt policies to curtail unnecessary exposure to radiation. The DRLs from the current study were 19.6 Gy·cm² for CAG; 49.8 Gy·cm² for PCI; and 72 Gy·cm² for CAG+PCI, considerably lower than the reference limits of other international studies (Supplementary Table 2 and Supplementary Table 3). Various factors could have contributed to this. Indians with cardiovascular disease are known to have a lower BMI than other ethnicities22. Most of the reference studies were much older; hence, this study might have had the benefit of improved radiation awareness, better experience of the operators, and recent advances in technical equipment.
Limitations
The current study has some important limitations. Radiation dose measurements were restricted to the three selected procedures (CAG, PCI, CAG+PCI) and hence no reference values can be deduced from this study for other catheterisation procedures. Detailed technical factors such as field of view, collimation, source-to-image distance and angulations have not been monitored. Lesion complexity and operator experience were not considered. There is no follow-up of patients who have received high radiation doses and the adverse effects of these high doses have not been reported.
Conclusions
DRLs for diagnostic and interventional coronary angiography procedures in India were calculated in this study. Despite variations across centres, radiation doses from a selection of tertiary cardiac care centres using similar equipment are comparable and are in the low range with reference to international standards. The establishment of these DRLs can be used as a benchmark for new or similar catheterisation laboratories.
Impact on daily practiceThe current study provides preliminary radiation exposure reference levels for commonly performed coronary procedures in India. This may serve as a reference for evaluation of radiation dose in individual catheterisation laboratories, to adapt policies and practices to improve their radiation doses. |
Acknowledgement
The authors thank Varun Gopinathand Bhavani who provided support in this study.
Funding
This work was supported in part by a GE Healthcare grant.
Conflict of interest statement
V. Subban has received an institutional research grant from GE Healthcare. S. Amelot is a GE Healthcare employee. The other authors have no conflicts of interest to declare.
