Introduction
When coronary angiography is used to assess for coronary artery disease, it is limited by the fact that it is a luminogram and is often dependent on specific angles of the recordings of angiographic sequences1. Intravascular ultrasound (IVUS) on the other hand, by virtue of providing a cross-sectional analysis, is better poised to offer more accurate and reproducible measurements of vessel and lumen diameters2. Assessment of these coronary dimensions is essential in determining the optimal device size to be used during percutaneous coronary intervention (PCI).
Left main coronary artery disease is a high-risk lesion subset and most recent studies have favoured coronary artery bypass grafting as the treatment of choice34. With the increasing understanding of anatomy and the increasing accuracy of dimension measurements, it is possible that outcomes of left main PCI can be optimised, as has been shown in various IVUS-guided studies5.
In this study, we aim to describe the characteristics of angiographically normal and insignificantly obstructed left main stem coronary arteries (LMS) using IVUS guidance on a mixed Indian population. The characteristics studied included reference diameter, luminal diameter, reference vessel area (RA), luminal area (LA) and calculated plaque burden. We also aim to show the degree of atherosclerotic involvement in what is perceived as an angiographically normal left main artery. This, we believe, will help define landing zones for future PCI.
Methods
This is a single-centre observational study and data were extracted from 198 consecutive patients who underwent PCI for left anterior descending (LAD), circumflex, or any of the left coronary branches excluding the left main artery, for which an IVUS pullback sequence of the LMS was available.
Objectives
- To determine reference vessel and luminal dimensions of the left main stem artery using IVUS in a subgroup of patients with either a normal LMS or one with insignificant disease as determined by coronary angiography
- To define the extent of atherosclerotic involvement in the left main stem occurring without luminal compromise and to assess its dimensions with respect to age, gender, body surface area, diabetes mellitus, hypertension and other variables.
Study population
This retrospective observational study is from a single centre involving 198 consecutive patients who underwent IVUS-guided PCI in the left anterior descending and/or the left circumflex artery or any of the left coronary branches over a 2-year period from 2019 to 2020, where a pullback sequence was available of the left main stem artery on IVUS. Patients with angiographically-assessed left main stem artery stenosis >30% were excluded from the study. As a result, the IVUS-guided analysis was performed on 140 patients after exclusion. We defined angiographically normal vessels as those with no evidence of any diameter change across the length of the left main artery in 2 angiographic views. Lesions with angiographically insignificant obstruction were described as those with at most a 30% reduction in diameter of the left main in at least 1 worst angiographic view.
All procedures were performed in accordance with the norms of the hospital with due consent. Use of dual antiplatelet agents, intravenous unfractionated heparin and other adjunctive pharmacological agents was as per guideline-based best practices. Activated clotting time was targeted between 250 to 300 seconds6. Prior to IVUS, all patients were given intracoronary 50 mg nitroglycerin aliquots for complete vasodilation.
IVUS was performed using the OPTICROSS 6 (40 MHz) or OPTICROSS HD (60 Mhz) (Boston Scientific) with automated pullbacks. All IVUS runs were obtained at 0.5 m/sec from a disease-free segment distally in the artery back to the proximal or ostial left main and back to the guiding catheter. All images were analysed with the Polaris Imaging System (Boston Scientific) and cross-checked with OsiriX software (Pixmeo).
Data collection and variable generation
Demographic and coronary artery data for 140 patients were collected and the body surface area (BSA) of each patient was calculated.
We calculated the reference diameter (RD), luminal diameter (LD), RA, LA, and plaque burden (PB) for each patient, as shown in Figure 1.
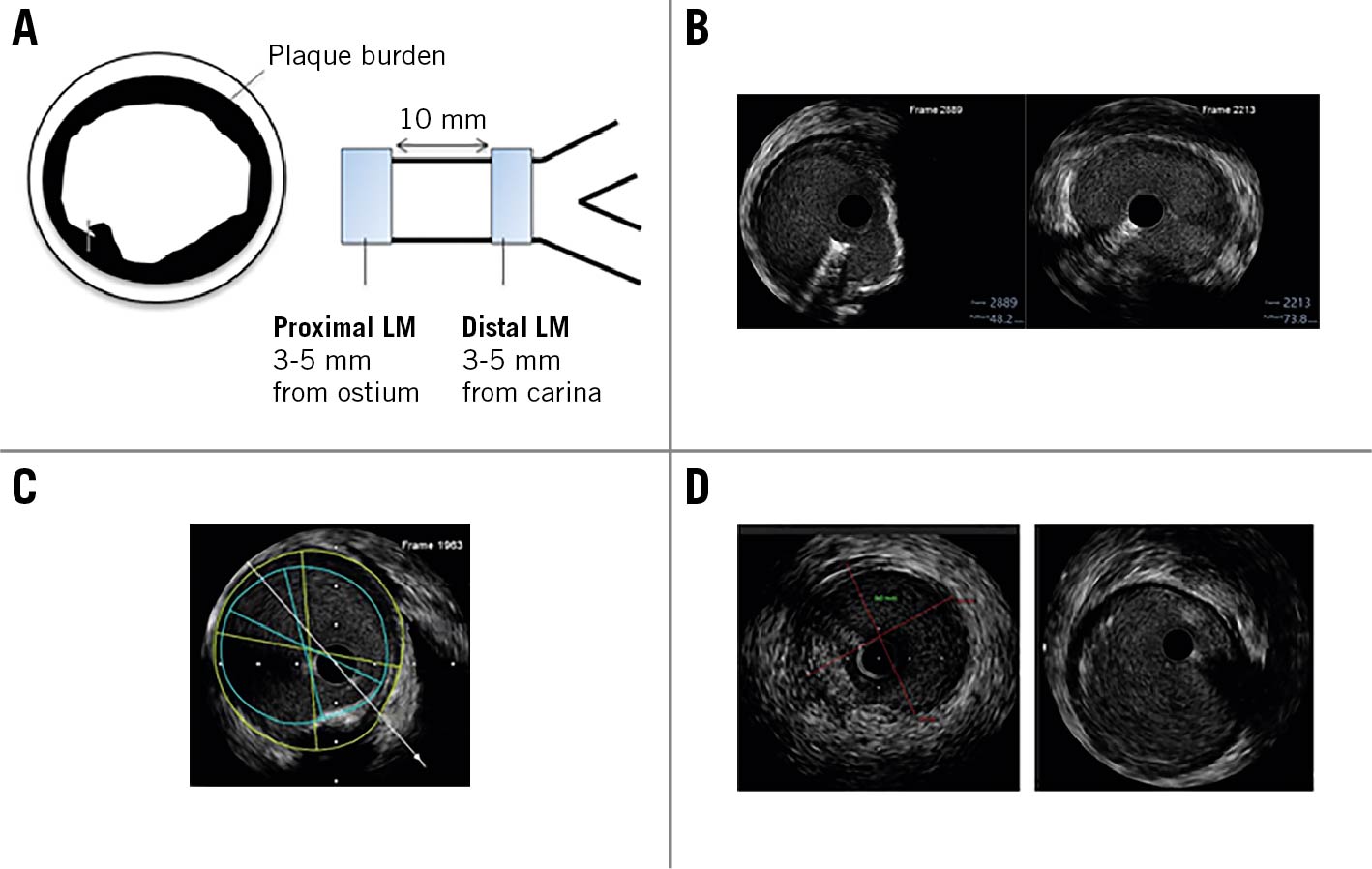
Figure 1. Measurements and images taken for the study. A) Schematic representation of plaque burden and proximal and distal left main arteries. If the left main length was less than 10 mm, only the distal left main diameter was taken. Plaque burden was calculated as (RA- LA)/RA*100. B) The left-hand image represents an angiographically insignificantly diseased left main artery showing a plaque from the 1 o’clock to 6 o’clock position. The right-hand image represents an angiographically normal left main artery. C) Diagrammatic representation of measurements taken for the study. The green and blue circles represent the RA and LA, respectively, and the green and blue lines represent the reference vessel diameter and lumen diameter, respectively. D) Left main image resolution in OPTICROSS 6 (40 MHz) (left) and OPTICROSS HD (60 MHz) (right). LA: luminal vessel area; LM: left main; RA: reference vessel area
To calculate reference diameters, two readings each of the proximal reference diameter (PRd) and distal reference diameter (DRd) were collected as shown in Figure 1. An average of the readings was taken to give us the PRd and DRd. The reference diameter was then calculated by taking the average of the proximal and distal reference diameters for each patient. The same method was applied to calculate the mean luminal diameter, reference vessel area, luminal area and plaque burden. In patients with an LMS length of less than 10 mm, only distal diameters were obtained.
Statistical analysis
Statistical analysis was conducted using the statistical software for data sciences, Stata 14 (StataCorp). Pearson’s correlation and simple linear regression were used to find the correlation between diameter and demographics and comorbidities. Descriptive analysis for all variables was reported as mean (standard deviation) for continuous variables and frequencies for categorical variables. A simple linear regression was used to study the relationship between vessel diameter and body surface area.
Results
IVUS pullbacks of 140 patients, including 114 males and 26 females, were examined and the characteristics and distribution of comorbidities are shown in Table 1.
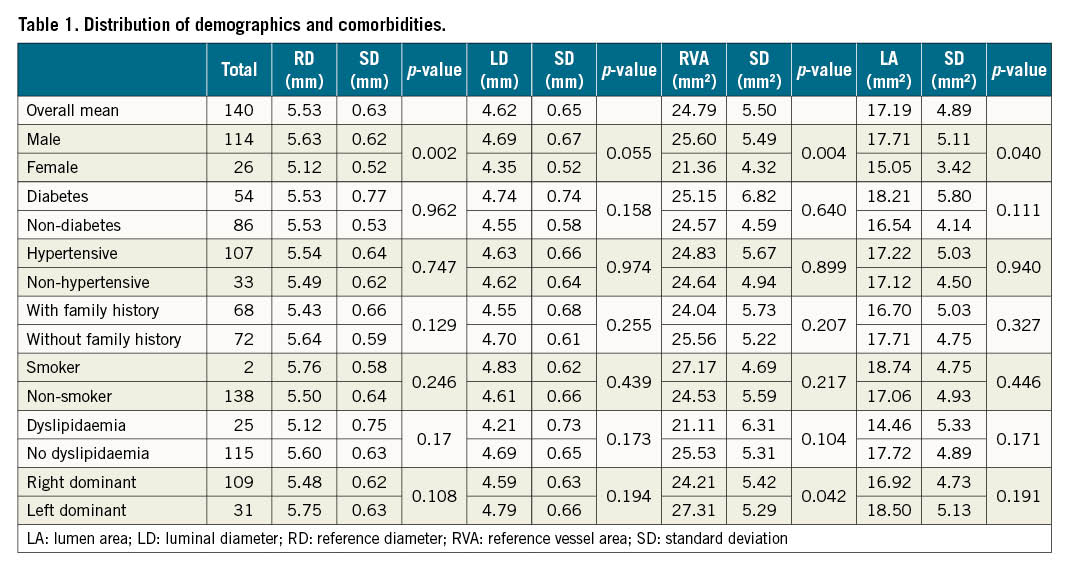
The IVUS-determined mean reference diameter of the left main artery was 5.53±0.63 mm and the mean luminal diameter was 4.62±0.65 mm. The mean reference vessel area was 24.79±5.5 mm2 and the luminal vessel area was 17.19±4.89 mm2. The distribution of the vessel diameters is shown in Figure 2.
A regression analysis performed to find the correlation between body mass index (BMI) and the diameters revealed a p-value of 0.212 for the reference diameter, 0.173 for the luminal diameter, 0.211 for the reference vessel area and 0.222 for the luminal area. The p-values derived between the body surface area (BSA) and diameters were 0.026, 0.055, 0.035 and 0.037 for RD, LD, RA and LA, respectively. Hence the body surface area showed a statistically significant correlation with the parameters.
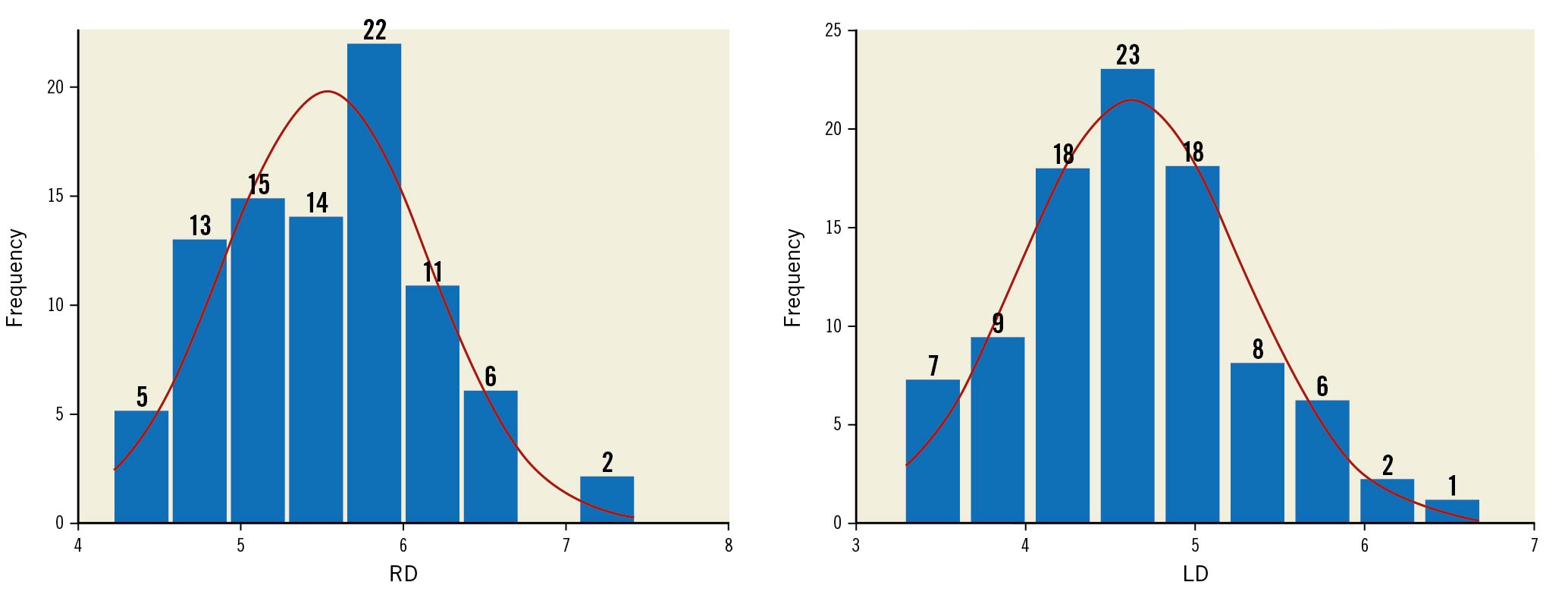
Figure 2. Distribution of reference diameter (RD) and luminal diameter (LD).
The reference vessel diameter sizes ranged from 4.3 to 6.5 mm with only 3 patients having a diameter greater than 6.5 mm and not a single vessel with a diameter less than 4 mm. The luminal diameter ranged from 3.3 mm to 5.8 mm with only 2 patients having a diameter greater than 6 mm.
The average diameter based on gender, comorbidities, smoking history, family history and dominance is shown in Table 1. Our results showed that the reference vessel diameter and the reference and luminal vessel areas are significantly smaller in females than in males (p-value=0.002, 0.004 and 0.04, respectively) (Figure 3). These parameters also showed a significant correlation with the body surface area (p-value=0.02, 0.03, 0.03, respectively) (Figure 4). In our present study the reference vessel area of the left main artery was significantly larger in left dominant as compared to right dominant circulation. No other parameter showed any significant correlation. In regression analysis, we did not find any significant difference in the size of the left main artery relative to age.
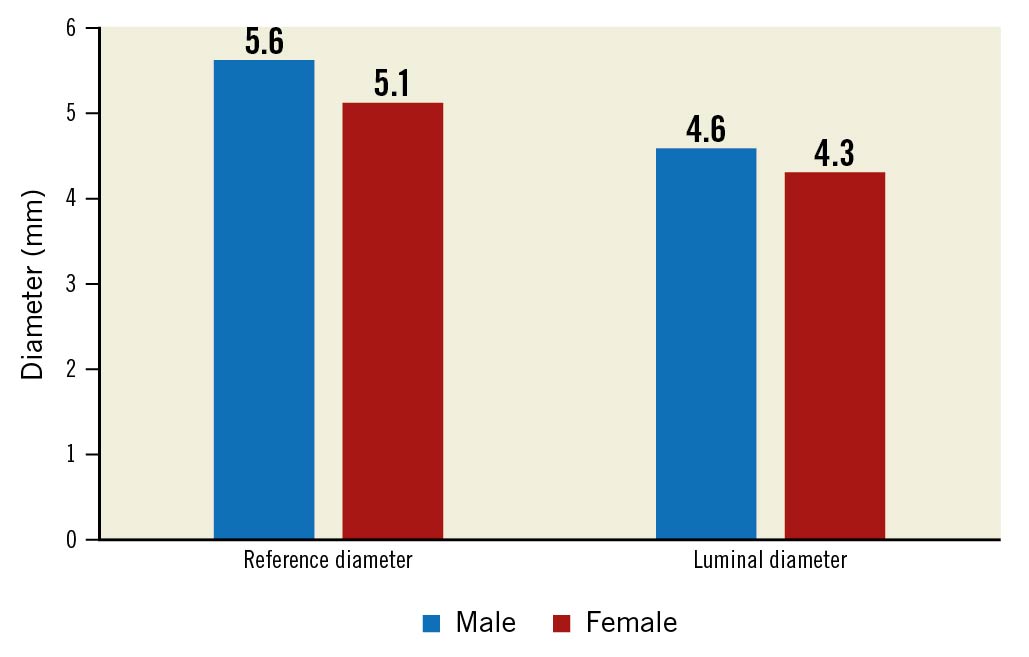
Figure 3. Reference diameter and luminal diameter in males and females.
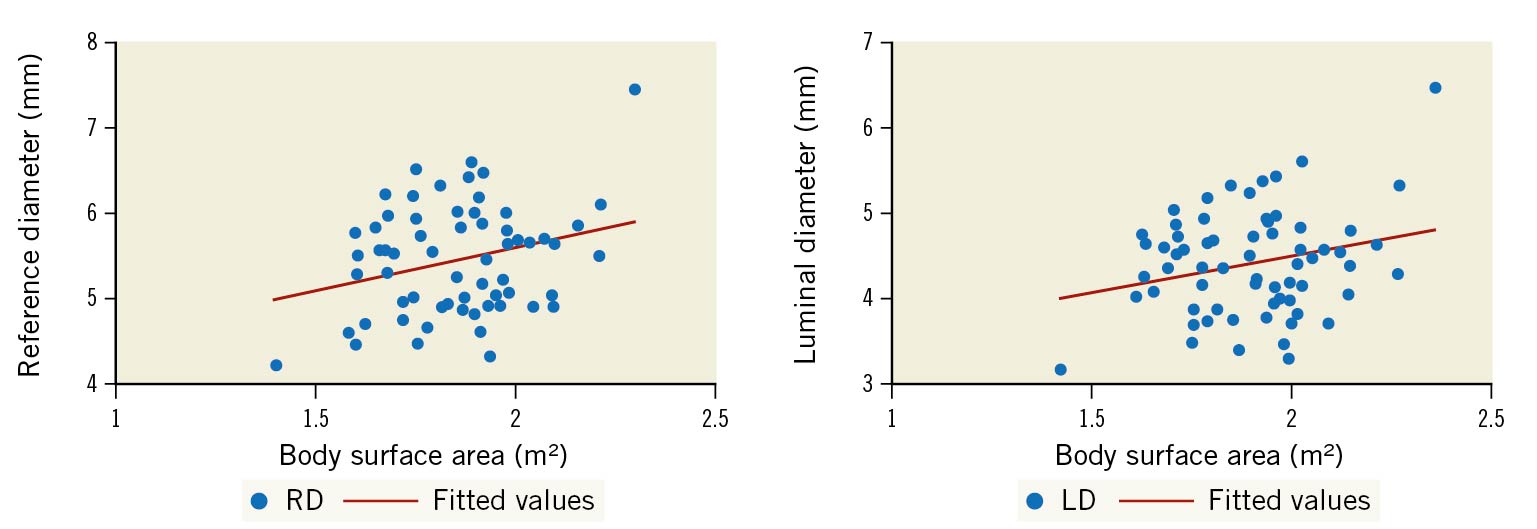
Figure 4. Linear correlation of reference and luminal diameters with body surface area. LD: luminal vessel diameter; RD: reference vessel diameter
The mean plaque burden was found to be 29.21% in patients with angiographically normal left main and 32.29% in patients with angiographically insignificant left main stenosis as depicted in Figure 5.
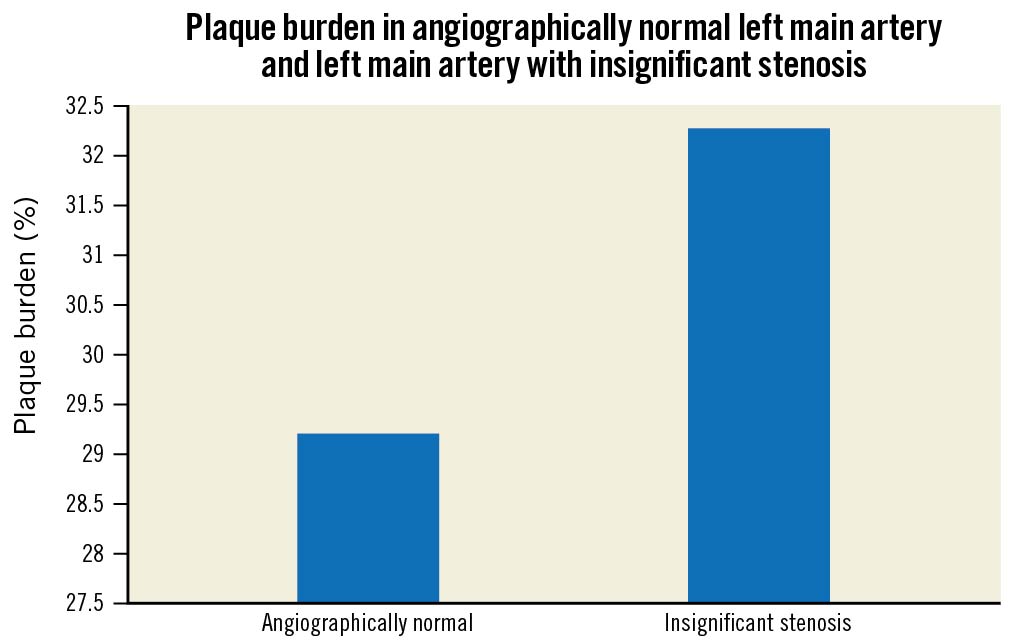
Figure 5. Distribution of plaque burden in angiographically normal left main artery and left main artery with insignificant stenosis. The mean plaque burden in an angiographically normal vessel ranged from 8-40% and from 20-50% in vessels with angiographically insignificant stenosis.
A simple linear regression was used to develop a model to elucidate the relationship between body surface area and vessel diameter. A one-unit increase in BSA leads to a 1.01 unit increase in reference vessel diameter and a 0.87 unit increase in luminal diameter.
Reference vessel diameter = 3.57+1.01 BSA
Luminal diameter = 2.95+0.87 BSA
The above formulae were tested for validation on 22 patients. The difference between interpreted and actual values averaged at approximately 0.54 mm for reference diameter and 0.24 mm for luminal diameter. This is shown in Figure 6.
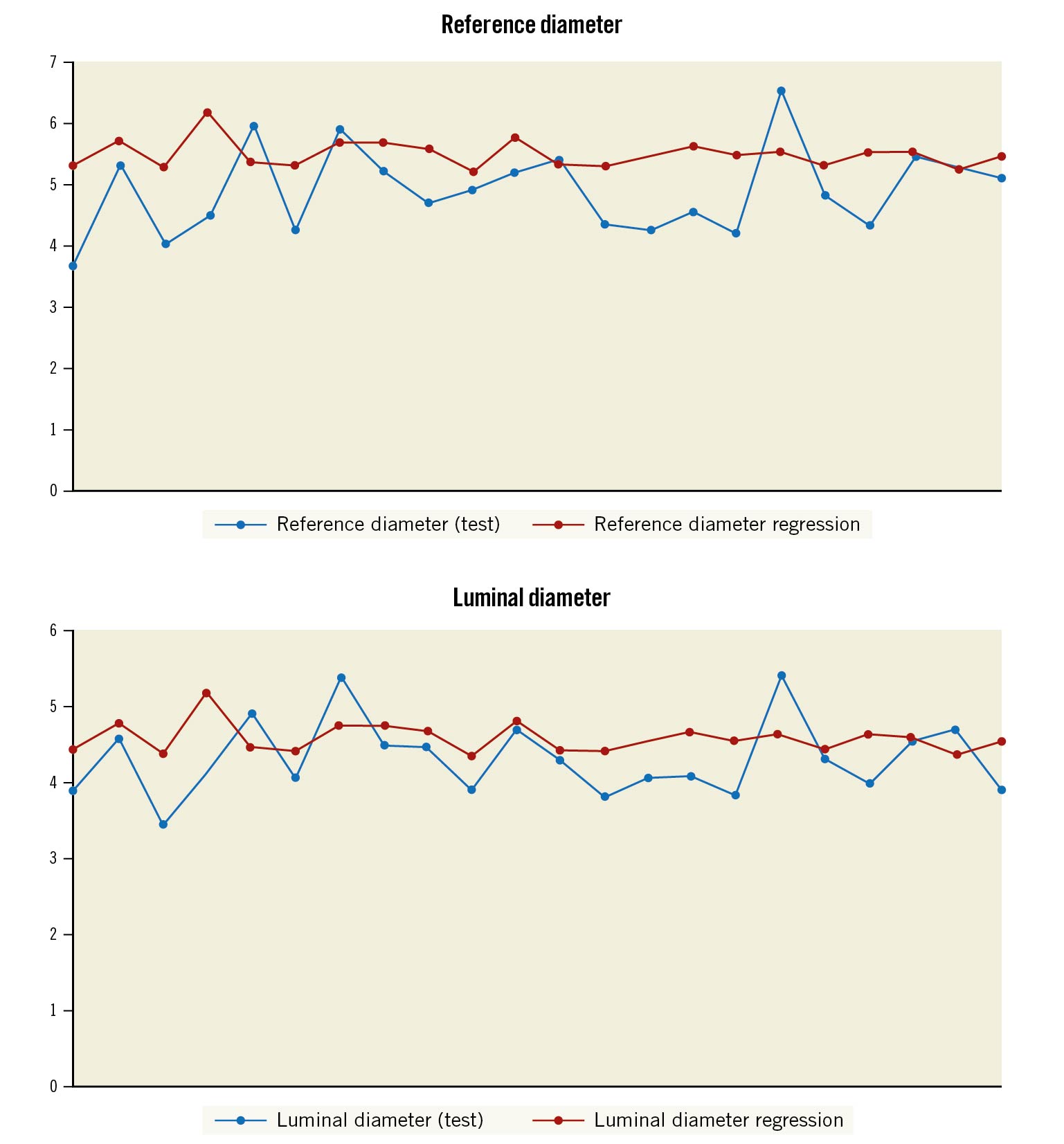
Figure 6. Actual reference and luminal diameters versus the values derived from the correlation equation.
Discussion
Our study found the mean reference vessel diameter of the left main stem in the Indian population to be 5.53±0.63 mm and the mean lumen diameter to be 4.62±0.65 mm. These absolute values are important parameters as they help identify the sizes needed for both stents and for the devices needed in the cath lab during coronary intervention involving the left main artery. It is important to note that very few patients in our study had a diameter less than 4 mm or greater than 6 mm. This observation is important in terms of the inventories of cath labs and will help cath labs with limited resources to economise.
A comparison of our study with other studies is shown in Table 2. The diameter of the left main vessel was similar to the findings of Goel et al7 who used IVUS to determine left main diameter in an Indian population. However, ours is the first study to have used OPTICROSS 6 (40 MHz) and OPTICROSS HD (60 MHz), which we believe to be superior technologies as compared to previous-generation IVUS and hence give a better understanding of the left main segment.
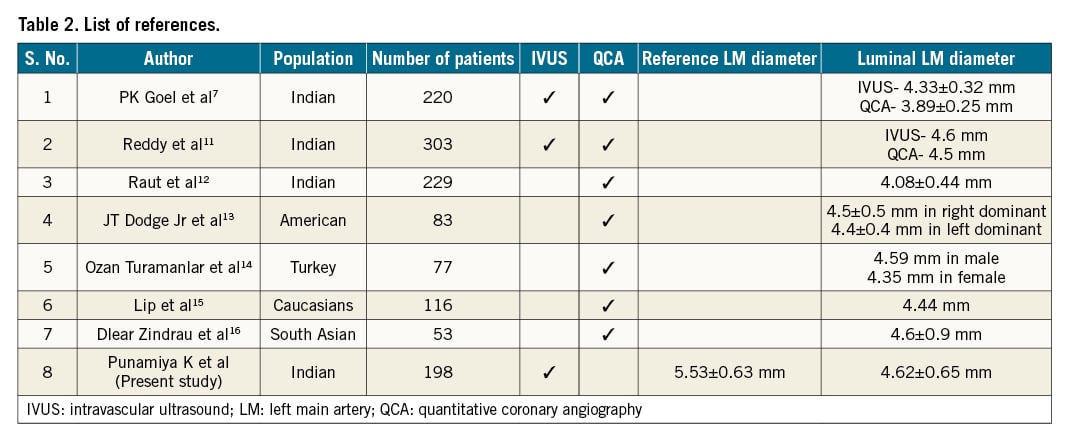
As shown in Table 2, we also found that the size of coronary vessels in the Indian population was on par with the size in other ethnicities. This is contrary to the previous understanding that Indians have a smaller coronary vessel diameter. This finding of similarity to Western populations has a significant impact on our ability to apply the same criteria used in the West on the Indian population.
Another important aspect of our study was the correlation described between the coronary vessel diameter and body surface area. To the best of our knowledge, no other study has described a correlation between body surface area and IVUS-determined size of the left main. This straight-line algorithm will help estimate left main diameters in patients from centres where IVUS is not routinely used. We plan to test the above formula on a larger number of patients in subsequent studies to test the validity of this algorithm.
Our study attempts to understand positive vascular remodelling in early atherosclerosis in the left main stem artery. The true vessel size, as determined by the reference diameter, is larger than the luminal diameter because of early plaque accumulation with positive vascular remodelling. We observed that a plaque burden of 32%±7.6% could exist with a well-preserved lumen area. We consider this important, as it helps to establish that a plaque burden of less than 40% is a good landing zone while performing left main PCI, as the lumen in this group of patients is not yet uncompromised. To the best of our knowledge this is the first study to have calculated the plaque burden in an angiographically normal left main artery and a left main artery with insignificant stenosis.
It was our preliminary impression that the external elastic lamina was better visualised using the OPTICROSS HD (60 MHz) IVUS as compared to OPTICROSS 6 (40 MHz) as shown in Figure 1D.
Unlike the findings of Mosseri et al8 we did not find any difference in the size of the LMS between those with or without diabetes mellitus and the sizes were also similar in patients with or without hypertension and dyslipidaemia. We could not find any significant difference between smokers and non-smokers, which is in contradiction with the findings of Fried et al9. Family history also does not have an impact on the size of the left main diameter. There was no change in the diameter of the left main artery relative to age.
Similar to the results of Dhall et al10, we found artery sizes to be significantly smaller in females than males. As described in previous studies, this is possibly because of the smaller body surface area of females as compared to males.
Limitations
Our study has certain limitations. Notably, a limited number of females were included in the study. Moreover, it was a single-centre study that may not be representative of the population as a whole, and it included a limited number of patients overall. It is important to note that despite our best efforts, we could not visualise the left main ostium in a third of the patients. A prospective study to validate our model based on the BSA of a larger number of patients is underway.
Conclusions
- The mean reference and luminal diameters of the left main artery in the Indian population are 5.53±0.63 mm and 4.62±0.65 mm, respectively. This is on par with the size of the left main in other ethnicities.
- The vessel compensates for up to 40% of plaque burden with vessel remodelling. Hence, a plaque burden of 40% is a good landing zone for stent deployment.
- The quality of images obtained by OPTICROSS HD was superior to the image quality with OPTICROSS 6.
- We derived a linear correlation between body surface area and left main artery diameter. The equation can be used to estimate vessel size in cath labs where IVUS is not available.
Impact on daily practice
We believe our study could help in improving the selection of device sizes during PCI, and hence lead to improved outcomes. It will help cath labs with limited resources to economise and to streamline their inventories.
Our study also sheds light on vessel remodelling and gives a better idea of landing zones for stents during PCI. The correlation equation derived in the study can be gainfully used in understanding left main and device sizes in cath labs where IVUS may not be regularly used.
The understanding of positive vascular remodelling defines a good landing zone for deploying stents during PCI.
Acknowledgements
We would like to acknowledge the contribution of Sanya Jha for statistical analysis and interpretation in this study.
Conflict of interest statement
The authors have no conflicts of interest to declare.
