Tricuspid regurgitation (TR) is an independent predictor of increased mortality1. Recently, transcatheter edge-to-edge repair (TEER) of the tricuspid valve using the TriClip (Abbott) has been studied in the TRILUMINATE Study2. In this paper, we summarise our 6-month follow-up experience after tricuspid TEER in a real-world setting emphasising fluid management and nutritional aspects.
For the present study, 33 consecutive patients were prospectively recruited between July 2020 and January 2021 with a planned 6-month follow-up using the first-generation TriClip system. To avoid a learning curve-related effect, patient recruitment started after the first five procedures. All patients met the following inclusion criteria: a) New York Heart Association (NYHA) Class ≥II; b) tricuspid regurgitation ≥grade 3; c) no concomitant, treatable severe cardiac disease; d) further clinical signs of tricuspid regurgitation, such as peripheral oedema; e) interdisciplinary Heart Team decision favouring an interventional approach. TR was quantified according to the five degrees grading from mild to torrential3 (Mild=1, Moderate=2, Severe=3, Massive=4 and Torrential=5).
Cardiovascular magnetic resonance imaging (CMR) was electrocardiogram (ECG)-gated and with a breath-hold using a 1.5T MAGNETOM Aera (Siemens). Body hydration was estimated with a bioelectrical impedance analysis. The study was approved by the local ethics committee.
The mean age of the patients was 78±6 years, and 67% were female. NTproBNP levels were elevated, with a median of 2,382 pg/ml (1,212-5,062). The patients had a median logistic EuroSCORE of 13.2 (9.4-20.1) and EuroSCORE II of 5.5 (3.9-9.5). Of the 33 patients recruited for this study, 26 patients had their 6-month follow-up visit. Five patients declined further participation due to the COVID-19 pandemic, and two patients passed away.
All 33 patients were successfully treated with TEER, using the “clover technique” in 25 cases (at least one anteroseptal and one posteroseptal clip) (Figure 1A – Figure 1D).
In-hospital mortality was 0%. Six-month mortality was 6%. No relevant procedural complications were noted, such as myocardial infarction, stroke, access-site bleeding, pericardial haemorrhage, infection or emergency surgery.
After 6 months, the reduction of TR was zero degrees for two patients, one degree for 10 patients, two degrees for 10 patients and three degrees for four patients. The dose of diuretics was not increased in any patient between admission for the procedure and 6-month follow-up. Nevertheless, weight significantly decreased (76.1±16kg versus 72.6±15kg; p=0.024) (Figure 1E) and body hydration was significantly lower after 6 months (81.5±5.9% versus 77.2±4.5%; p=0.005) (Figure 1F). Interestingly, serum albumin levels had significantly increased after 6 months (3.7±0.5 g/dl to 4.3±0.4 g/dl; p<0.0005) (Figure 1G), which was a sign of reduced intestinal congestion and improved nutrition, and most likely contributed to the reduced hydration levels. These findings corresponded to a significantly improved NYHA Class at follow-up from 2.9±0.6 to 2.3±0.7 (p=0.001).
Baseline and 6-month follow-up CMR data were available for 13 patients. The right ventricular (RV) end-diastolic volume index (RVEDVI) at baseline was 103+26 ml/m² and decreased to 86±17 ml/m² (p=0.009) (Figure 1H).
In this early follow-up study of real-world patients receiving tricuspid TEER, TR and heart failure symptoms consistently and significantly improved after 6 months. More interestingly, weight and body hydration showed a significant reduction. In accordance with these findings, serum albumin levels showed a significant increase, hinting at lower venous congestion in the intestinal tract with improved nutrition and improved body-water to muscle-and-fat ratio. CMR data of reduced RVEDVI show early signs of a reverse remodelling.
This study is limited by the small sample size and single-centre design. Data have to be interpreted cautiously.
Tricuspid TEER can improve parameters related to the pathophysiology of TR after 6 months.
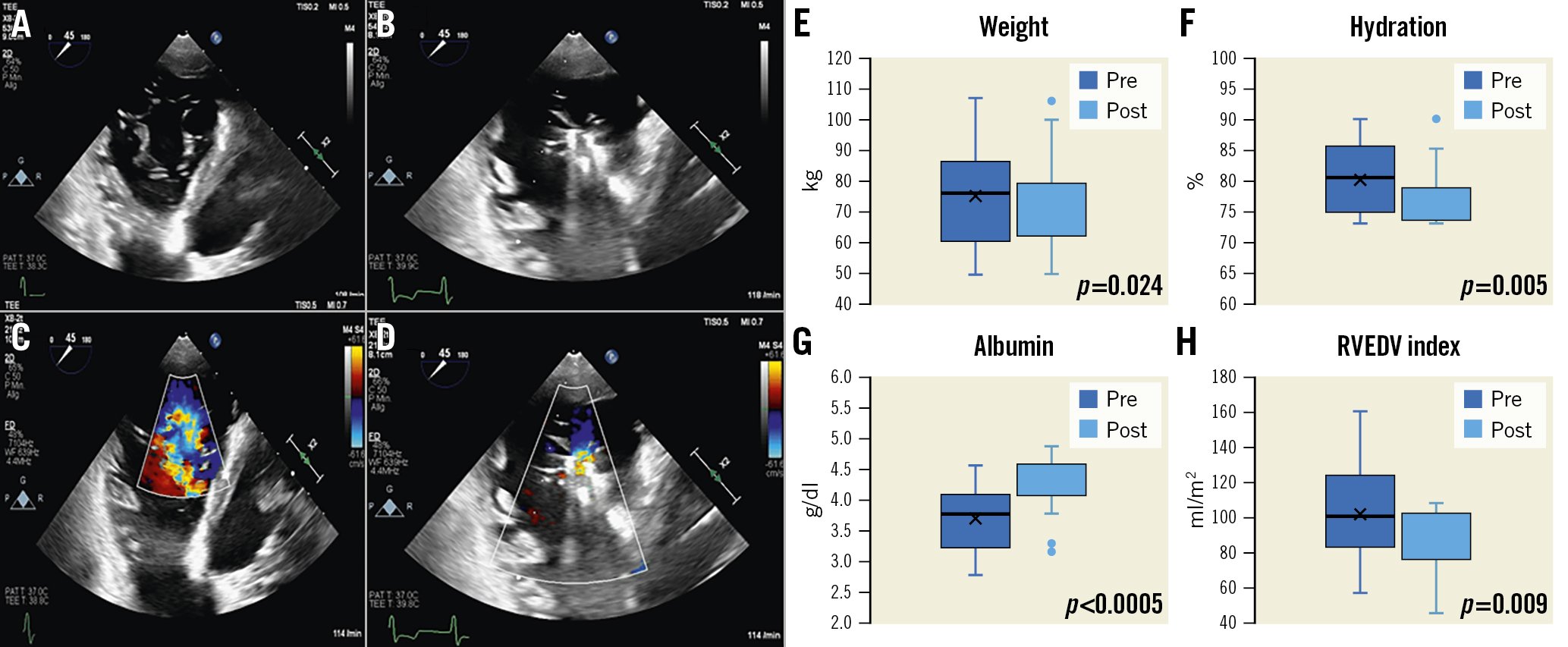
Figure 1. Results after tricuspid TEER. Left: transgastric views of a tricuspid valve clip implantation (A,C) and after implantation of one anteroseptal and posteroseptal clip (the“clover technique” [B,D]). Right: 6 months after TEER, significant decrease in weight (E), hydration (F) and RVEDV index (H) and significant increase in serum albumin (G). RVEDV: right ventricular end-diastolic volume; TEER: transcatheter edge-to-edge repair
Conflict of interest statement
P. Nikolai has received speaker and proctor honorariafrom Abbott. R. Bekeredjian reports research grant support from Abbott. The other authors have no conflicts of interest to declare.
