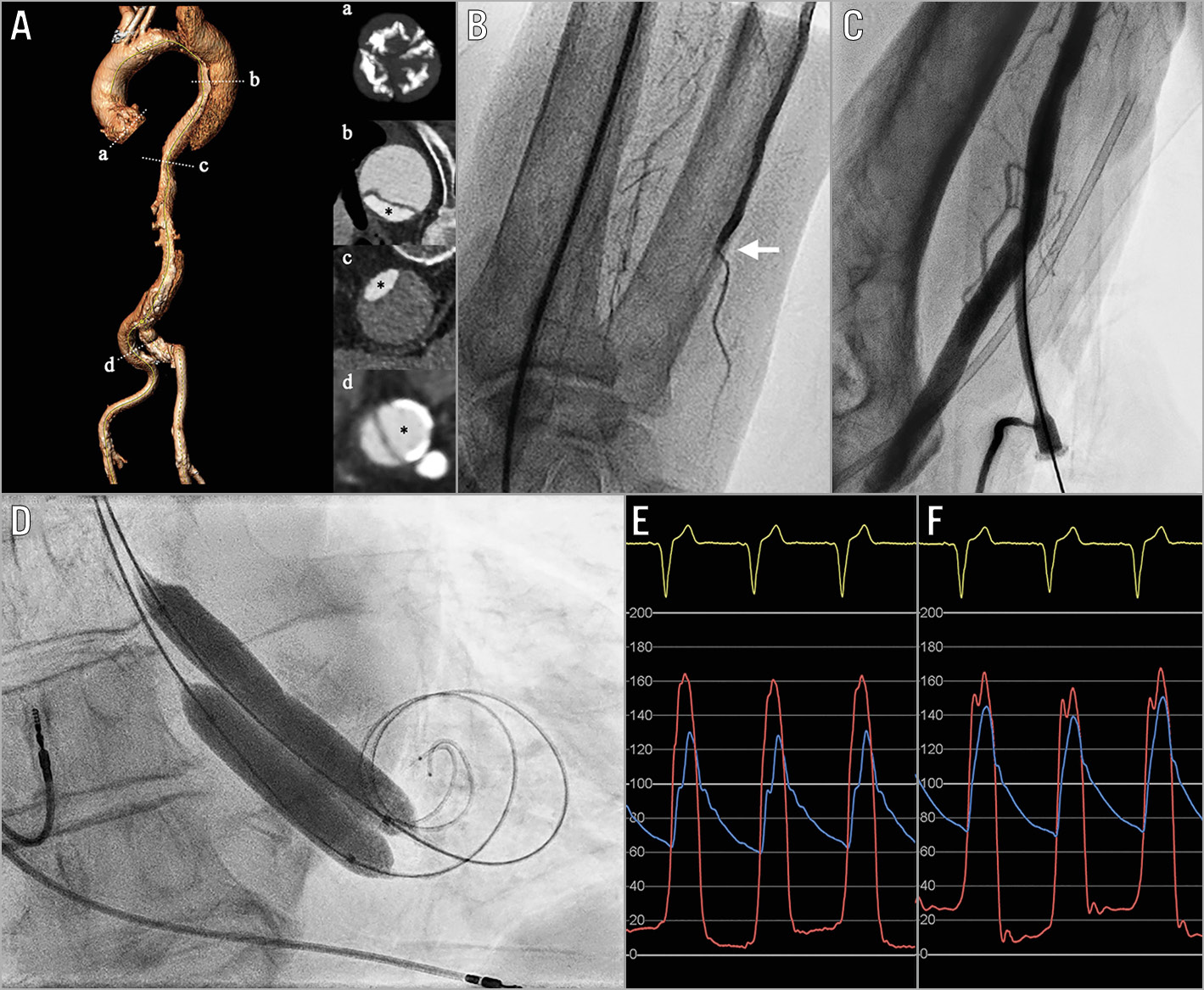
Figure 1. BAV with two simultaneous balloons via ipsilateral transradial and transbrachial access. A) Chronic type B aortic dissection extending from the left subclavian artery to the right iliofemoral artery: (a) severely calcified aortic valve; (b) aortic arch; (c) descending thoracic aorta; (d) right iliofemoral artery. Asterisk (*) indicates the true lumen. B) Patent right radial artery and occluded right ulnar artery (white arrow). C) Right brachial artery access. D) BAV with two simultaneous balloons. E) & F) Pre- and post-BAV invasive peak-to-peak gradient. BAV: balloon aortic valvuloplasty
Balloon aortic valvuloplasty (BAV) continues to play a role in the management of severe aortic stenosis (AS) in selected patients, either as a bridge to percutaneous or surgical aortic valve replacement or as a destination therapy. BAV is usually performed via transfemoral access but, when impossible, transradial approaches have been utilised – unilateral access with a single compliant balloon or bilateral access with two simultaneous peripheral balloons.
A frail 84-year-old male with severe AS presented with recurrent pulmonary oedema (Figure 1). He was declined surgical or transcatheter aortic valve replacement due to poor prognosis and an inoperable chronic type B aortic dissection extending from the left subclavian artery to the right iliofemoral artery. Palliative BAV was considered but aortic dissection precluded safe transfemoral or left transradial access. The intended strategy was therefore a simultaneous inflation of two 12 mm peripheral balloons (mean annulus diameter 26.8 mm on multislice computed tomography) via unilateral right radial and ulnar arterial access (7 Fr). However, the ulnar artery was occluded; a second access was achieved via an ultrasound-guided right brachial arterial puncture (vessel diameter 9.1 mm on ultrasound). Weight-adjusted unfractionated heparin was administered (activated clotting time [ACT] 330 sec), two Safari™ wires (Boston Scientific, Marlborough, MA, USA) were positioned in the left ventricle, and two 12 mm POWERFLEX® Pro balloons (Cordis, Miami Lakes, FL, USA) were simultaneously inflated under rapid ventricular pacing “on-the-wire”. The invasive peak-to-peak gradient decreased from 40 to 17 mmHg without an increase in aortic regurgitation. Protamine sulphate was administered (ACT 109 sec) and then compression haemostasis was used. Prolonged manual compression was needed for the brachial access. The patient was discharged on a direct oral anticoagulant due to atrial fibrillation and had no further admissions at three months.
This case demonstrates the feasibility of an ipsilateral approach for BAV with two simultaneous balloons in selected cases. Meticulous procedural planning and rigorous haemostasis management are crucial.
Conflict of interest statement
D. Mylotte is a consultant for Medtronic, Boston Scientific, and MicroPort, and declares personal fees from Medtronic, Boston Scientific, and MicroPort. The other authors have no conflicts of interest to declare.