Yusuke Hosokawa, Koji Kato, et al
The three most common underlying mechanisms of acute coronary syndrome (ACS) are believed to be plaque rupture, plaque erosion and, least common, a calcified nodule. Although treatment of ACS mainly consists of catheter-based reperfusion using a coronary stent, it remains under discussion whether deployment of a coronary stent is necessary for a culprit calcified nodule, particularly
when coronary flow is preserved.
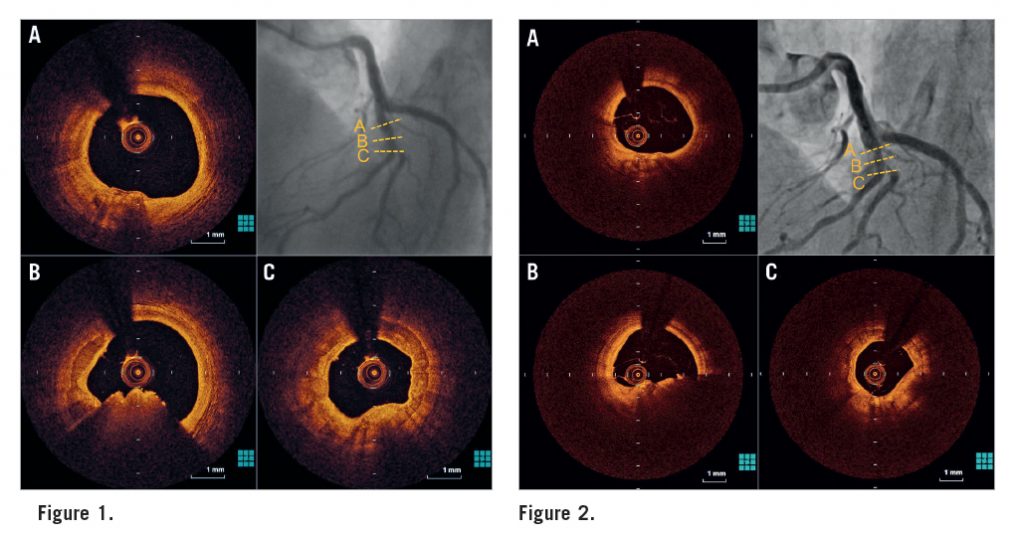
A 75-year-old man with ST-elevation myocardial infarction (STEMI) was referred to our hospital. He had a history of hypertension and dyslipidaemia. Emergency coronary angiography revealed a moderately stenotic lesion in the mid left anterior descending coronary artery (LAD) with a filling defect (Moving image 1). Protrusion of calcium with an overlying thrombus was observed by optical coherence tomography (OCT), but neither plaque rupture nor erosion was detected (Figure 1, Moving image 2). The diagnosis of STEMI caused by a calcified nodule was made. We avoided coronary stent deployment and initiated dual antiplatelet therapy (DAPT) because the coronary flow was preserved. Follow-up CAG three months later showed mild stenosis in the mid LAD (Moving image 3) and OCT revealed a residual thrombus at the same site (Figure 2, Moving image 4). We then decided to treat the lesion with a coronary stent (Moving image 5), since the thrombus had persisted, despite three months of DAPT.
Calcified nodules are characterised by disruptive nodular calcifications protruding into the lumen and known to be the cause of coronary thrombosis. Because the pathophysiological process of a calcified nodule is different from that of plaque rupture or erosion, tailored treatment is required when this morphology is observed at a culprit lesion. In our case, we initially tried to treat this calcified nodule with DAPT, but, as a result, avoiding stent implantation failed to obtain the satisfactory morphological outcome and we finally implanted a coronary stent. However, it is controversial whether this decision was correct because there is no evidence concerning the treatment of calcified lesions with persistent thrombus resistant to DAPT.
Supplementary data
[/custom_font]
Moving image 1. Coronary angiography showed a moderately stenotic lesion in the mid left anterior descending coronary artery with a filling defect.
Moving image 2. Optical coherence tomography showed protrusion of calcium with an overlying thrombus.
Moving image 3. Follow-up coronary angiography at three months showed mild stenosis in the mid left anterior descending coronary artery.
Moving image 4. Follow-up optical coherence tomography at three months revealed a residual thrombus at the same site.
Moving image 5. A coronary stent was implanted in the lesion.