Left ventricular pseudoaneurysm (LVP) is a rare but life-threatening complication, mostly reported secondary to myocardial infarction (MI) or cardiac surgery1. LVP is contained by adherent pericardium or scar tissue, with no myocardial tissue, and becomes a nidus for thrombus formation23. Emergent surgical repair or a percutaneous device with minimal invasion are the available treatment options. We herein report a case of the percutaneous closure of an LVP with a vascular plug.
A 70-year-old female with diabetes mellitus and hypertension suffered from an inferolateral MI that was treated by coronary angioplasty with stenting to the right coronary artery. She presented with progressive worsening dyspnoea for 3 weeks. Investigations revealed only raised brain natriuretic peptide levels (1250 pg/dl); echocardiography showed depressed left ventricular (LV) function (LV ejection fraction 35%) with a large pseudoaneurysm from the mid-part of posteroinferior wall of the LV measuring 36×33 mm with a neck of 12.3 mm. The cardiac computed tomography (CT) also confirmed the size.
The patient was stabilised with optimal medical therapy, and various treatment options were discussed for LVP; the patient and family opted for closure by device. After general anaesthesia, access was obtained to the bilateral femoral arteries and the left femoral veins; an LV angiogram confirmed the location of the LVP. The neck of the LVP was crossed with a Terumo wire, and a multipurpose catheter which was exchanged with a 7 Fr delivery sheath over a double-length Amplatzer Super Stiff wire (Boston Scientific). An Amplatzer Vascular Plug type II (20 mm; Abbott) was selected; two distal discs were deployed in the LVP cavity, and the third disc was released on the LV side after confirming the position on the LV angiogram and transthoracic echocardiogram. The patient was started on dual antiplatelet therapy with standard antifailure medication. At 4-month follow-up, the patient was stable with no active cardiac symptoms.
A ventricular pseudoaneurysm, unlike a true aneurysm, is enclosed by the pericardium, pericardial adhesions or thrombi13; most LVPs develop after MI or cardiothoracic surgery. If untreated, the risk of LVP rupture within the first year is 30% to 45%234. In a case series, the most common site for the development of a pseudoaneurysm after MI was on the inferior or posterolateral wall (in 82% patients)23. Although surgical repair is the preferred treatment, it is associated with 20% mortality4.
Transthoracic echocardiography and transoesophageal echocardiography are 26% and 75% effective in making a definitive diagnosis, respectively5. Cardiac CT and cardiac magnetic resonance imaging are helpful in differentiating LVP from true aneurysms, and they have a reported sensitivity of 100%5. Medical treatment has been advocated in the past for patients with a higher risk of morbidity and mortality following surgery. It is reported that the rupture risk in LVPs increases to 48% when managed with medical treatment alone4. Percutaneous approaches can be utilised for smaller pseudoaneurysms but there is a small risk of rupture, thromboembolism or cardiac failure. Although multiple devices, like septal occluders and duct occluders, are used by different operators, the choice of device is best decided by the primary operator. In our case, we chose the Amplatzer Vascular Plug II for its unique design and smaller profile. We were able to occlude the neck of the LVP completely, with no residual flow across it, and this was confirmed with different imaging modalities. The vascular plug can be a feasible alternative to other devices in patients with comorbidities and high surgical risk.
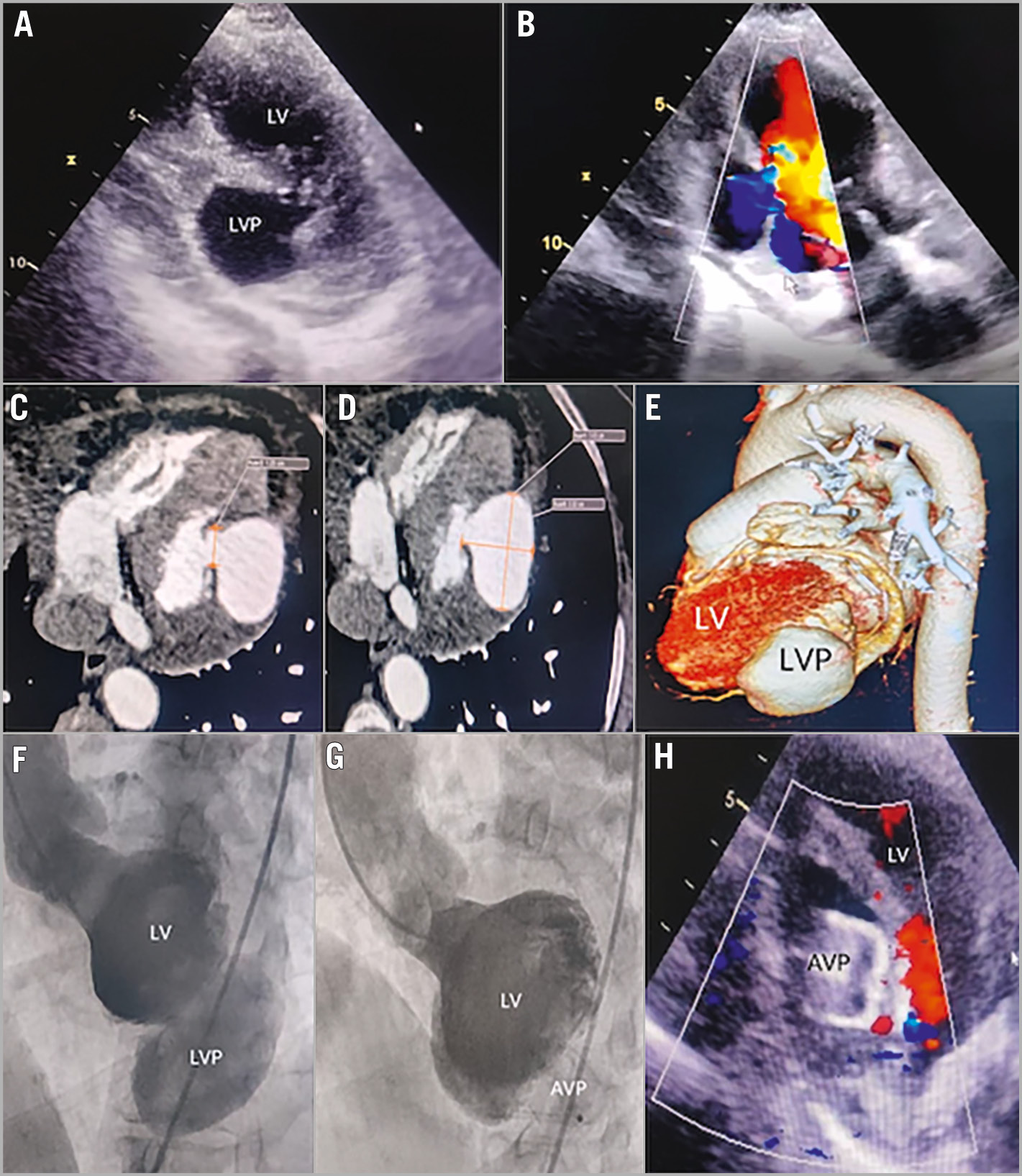
Figure 1. Percutaneous device closure of left ventricular pseudoaneurysm. Transthoracic echocardiographic images for LVP. An orthogonal view (A) and parasternal long-axis view with colour Doppler (B) show a large posteroinferior LVP. Cardiac CT cross-sectional images show an LVP with a neck measuring 12.3 mm (C) and dimensions of 36×33 mm (D). The three-dimensional rendered CT image (E) shows the posteroinferior location of the LVP. The LV angiogram (LAO view) shows a large LVP from the posterolateral surface (F) which was completely closed with an AVP, with no residual flow on the angiogram (G). The follow-up transthoracic echocardiogram (H) shows a good position of the AVP with no residual flow. AVP: Amplatzer Vascular Plug type II; CT: computed tomography; LAO: left anterior oblique; LV: left ventricle; LVP: left ventricular pseudoaneurysm
Conflict of interest statement
The authors have no conflicts of interest to declare.