An 80-year-old male patient with type II diabetes mellitus and chronic kidney disease (CKD; baseline creatinine 2.16 mg/dL; estimated glomerular filtration rate 20 ml/min/1.73 m2) presented with non-ST-segment elevation myocardial infarction. He was referred for staged percutaneous coronary intervention (PCI) of a right coronary artery (RCA) aorto-ostial lesion (AOL) (Figure 1A, Moving image 1) following PCI of a culprit lesion in the left anterior descending artery (LAD). Echocardiography showed a left ventricular ejection fraction of 40% and hypokinesia of the LAD-dependent myocardium. We proceeded to perform a sheathless transradial PCI using a 7 Fr standard Judkins right 4.0 guide catheter with contrast-preserving techniques. Using the aortic calcification noted adjacent to the RCA ostium as a pointer, we confirmed proper ostial positioning of the catheter with electrocardiographic repolarisation changes after an injection of saline. The previous angiogram was used as a guide for wiring the RCA. Intravascular ultrasound (IVUS) was then performed showing a calcified AOL (Figure 1A). The lesion was dilated with a 3.5 mm scoring balloon and a 3.75 mm non-compliant balloon, and both balloons expanded fully and uniformly at 20 atm. A second (“floating”) guidewire was then placed in the aortic root followed by the positioning of a 3.5 mm x 34 mm drug-eluting stent across the lesion. An IVUS catheter was then advanced over the “floating” guidewire (Figure 1B), allowing us to adjust the stent position under live IVUS imaging so as to fully cover the ostium. The stent was then deployed and postdilated with a 4.0 mm non-compliant balloon inflated at 20 atm. Additional post-dilation of the stent covering the ostium and stent flaring was performed using a 4.5 mm non-compliant balloon inflated at 20 atm. An optimal PCI result was documented by IVUS and a single angiographic image using 3 ml of contrast medium (Figure 1C-Figure 1D–Figure 1E, Moving image 2, Moving image 3). Percutaneous coronary intervention of RCA AOLs still poses unique challenges and is associated with subsequent target lesion revascularisation (TLR) even when performed using new-generation drug-eluting stents1. Several anatomical reasons associated with a high risk of in-stent restenosis (ISR) are known to be prevalent in AOLs, such as fibrosis, calcification and thick muscular elastic tissue, all resulting in poor lesion distensibility and propensity for recoil. Further to these anatomical reasons, inaccurate stent placement, also known as geographical miss, has been associated with a threefold increase in ISR and TLR rates23. Geographical miss is diagnosed when any part of the circumference of the proximal stent edge is located proximal or distal to the aorto-ostial landing zone that is located within 1 mm proximal and distal to the aorto-ostial plane34. Furthermore, current practical recommendations advocate that stents in AOLs be deployed with 1-2 mm protruding into the aorta to ensure ostial coverage and to not hinder re-engagement of the vessel during future PCI5. Indeed, angiography-guided PCI of AOLs has been associated with 54% and 87% incidences of geographical miss detected by angiography and computed tomography angiography, respectively, partly because conventional angiography is inherently limited in accurately demarcating the true coronary ostium34. Furthermore, angiography-guided PCI of ostial lesions has been shown to be independently associated with use of a higher volume of contrast medium, that may potentially be particularly detrimental in patients at risk of contrast-induced nephropathy (CIN)6. Indeed, the risk of CIN in patients with severe CKD is high (26.6%) entailing an increased risk of adverse outcomes, including in-hospital death (9.6%)7. Consequently, the application of contrast-preserving techniques that would also ensure optimal stent positioning was imperative in our case. The “floating” IVUS technique herewith presented facilitated accurate aorto-ostial RCA stent positioning under the direct guidance of live imaging, therefore obviating the use of contrast medium, and potentially thereby helping to decrease the risk of TLR while simultaneously averting CIN and the associated increased morbidity and mortality. The successful application of this technique requires positioning the IVUS catheter in such a way as to clearly visualise the coronary artery ostium, followed by a slow and steady retraction of the stent towards the aorto-ostium until the proximal edge of the stent, recognised as a spherical echogenic structure with an acoustic shadow behind it, is visualised in the aorta immediately past the coronary artery ostium. Having the stent deployed in this position ensures complete stent coverage of the aorto-ostium, without excessive stent overhang into the aorta. Indeed, the application of this technique in our case resulted in an optimal stent location with the stent completely covering the aorto-ostium and having a part of the circumference of its proximal edge protruding about 1.5 mm into the aorta (Figure 1E), which is very much acceptable from a practical standpoint. 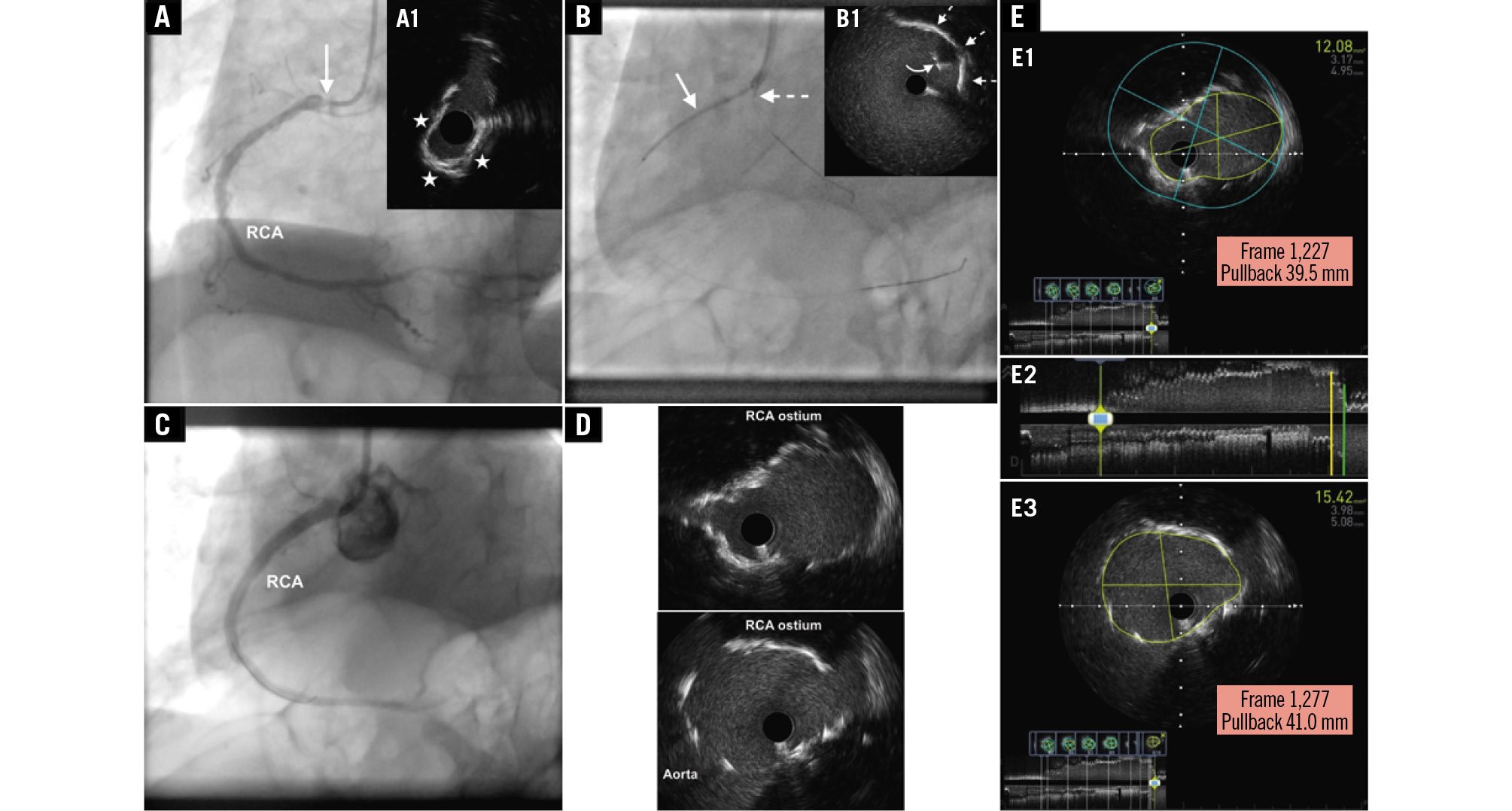
Figure 1. Conventional angiographic and IVUS images presenting the “floating” IVUS technique applied in the treatment of an aorto-ostial RCA lesion. A) Conventional angiographic image of the RCA at baseline (left anterior oblique 30° projection) depicting a high-grade ostial stenosis (arrow). Cross-sectional IVUS (60 MHz OptiCross catheter [Boston Scientific]) image (A1) depicting a severely narrowed ostium (minimal lumen area 3.5 mm2) due to a calcified lesion (calcium arc denoted by the asterisks). B) The stent is shown in position across the lesion (arrow). An IVUS catheter placed over a “floating” guidewire in the aortic root is also shown in such a position so that the transducer (dashed arrow) faces the ostium of the RCA. Cross-sectional IVUS image (B1) depicting the proximal edge of the stent (curved arrow) at the ostium of the RCA (dashed arrows), recognisable by its echogenic appearance with an acoustic shadow behind it, as opposed to a reverberation artefact, comprising arc-shaped, high-echoic lines appearing behind the proximal portion of the wrapped balloon and the balloon marker. C) Conventional angiographic image (left anterior oblique 30° projection) acquired at 30 frames per second depicting a good result after stenting the RCA lesion. D) Cross-sectional IVUS images from the RCA depicting optimal coverage of the ostium where the minimal stent area ranged between 12.0 mm2 and 15.0 mm2. E) Longitudinal view of the final IVUS recording (E2) showing complete stent coverage of the aorto-ostium (E1, corresponding to the cross-section marked with a yellow line in the longitudinal view) and a partially protruding stent (E3, corresponding to the cross-section marked with a green line in the longitudinal view) with a length of 1.5 mm (IVUS pullback speed: 1 mm/sec; frame rate: 30 frames/sec; see frame number and distance shown within the red rectangles in E1 and E3). IVUS: intravascular ultrasound; RCA: right coronary artery
Conflict of interest statement
A.Y. Andreou has no conflicts of interest to declare.

