Little is known about the downsides of oversizing with the WATCHMAN FLX (Boston Scientific) device. Here we present a case of impressive device deformation due to a reverse inside fold. Two-dimensional (2D) transoesophageal echography (TOE) alone may have missed this “origami” shape, but adding three-dimensional (3D) multiplanar reconstruction (MPR) imaging was effective in detecting it.
A 75-year-old male with persistent atrial fibrillation was scheduled to receive left atrial appendage (LAA) closure with the WATCHMAN FLX, due to a CHA2DS2-VASc score of 4 and a history of Bleeding Academic Research Consortium (BARC) Type 3 gastrointestinal bleeding. Preoperative contrast-enhanced computed tomography (CT) showed the LAA as having an anterior chicken wing shape, and the maximum coaxial diameter of the device landing zone was 21.3 mm (Figure 1A). We considered employing either a 24 mm or 27 mm WATCHMAN FLX device. Intraoperative 2D TOE showed 18.8 mm as the maximum ostial diameter. However, the diameter of the LAA orifice was smooth and wide, measuring 24.6 mm at 135° (Figure 1B). To avoid potential device dislodgement with a 24 mm device implanted proximal to the landing zone, a 27 mm device was selected instead. After the first deployment, the device was implanted proximal to the LAA ostium but did not meet the lower compression rate. We then tried a partial recapture and pushed the device further in with forward tension. After the second deployment, 2D TOE and angiography showed the device to be inadequately expanded (Figure 1C, Moving image 1). MPR by 3D TOE showed that half of one side of the device’s surface was folded into an inside reverse fold − resembling an origami crane head − and was overcompressed by 10.6 mm (39.2% of compression rate) (Figure 1D–Figure 1G, Moving image 2). The deformed device was recaptured without problem. We attempted another partial recapture but failed to meet the adequate compression rate. Finally, we switched to a 24 mm device. The removed 27 mm device showed no abnormality of the structure. The 24 mm device was well seated in the LAA after the first deployment, so we considered the deformation of the 27 mm device to be due to oversizing. The compression rate ranged from 21.3% to 25.8%. After confirming the PASS (position, anchoring, size, seal) criteria, we released the 24 mm device. The procedure was completed without any complications.
We present a rare case of an inside reverse fold of the WATCHMAN FLX device. Since device dislodgement is a fatal complication, device oversizing according to manufacturer recommendations seems to be common in clinical practice1. However, implantation of an oversized device may cause deformation of the device, especially on the side that is fixed. Pruitt et al proposed that a similar deployment complication can be caused by an acute angle between the catheter and LAA ostium2. In this case, we pushed the device with forward tension, which resulted in losing coaxiality and increasing the angle between the catheter and LAA ostium. During the 24 mm device implantation, we did not change the septal puncture location or the double curved sheath, so the angle between the sheath and the LAA alone cannot explain the cause of the deformation. This case report highlights that MPR of 3D TOE can show the entire surface of the device and prevent underestimation of device deformation, which cannot be identified with 2D TOE. The depressed surface of the device could lead to future device-related thrombus or peridevice leak, so it is important to check MPR with 3D TOE when you encounter an LAA closure device which is overcompressed.
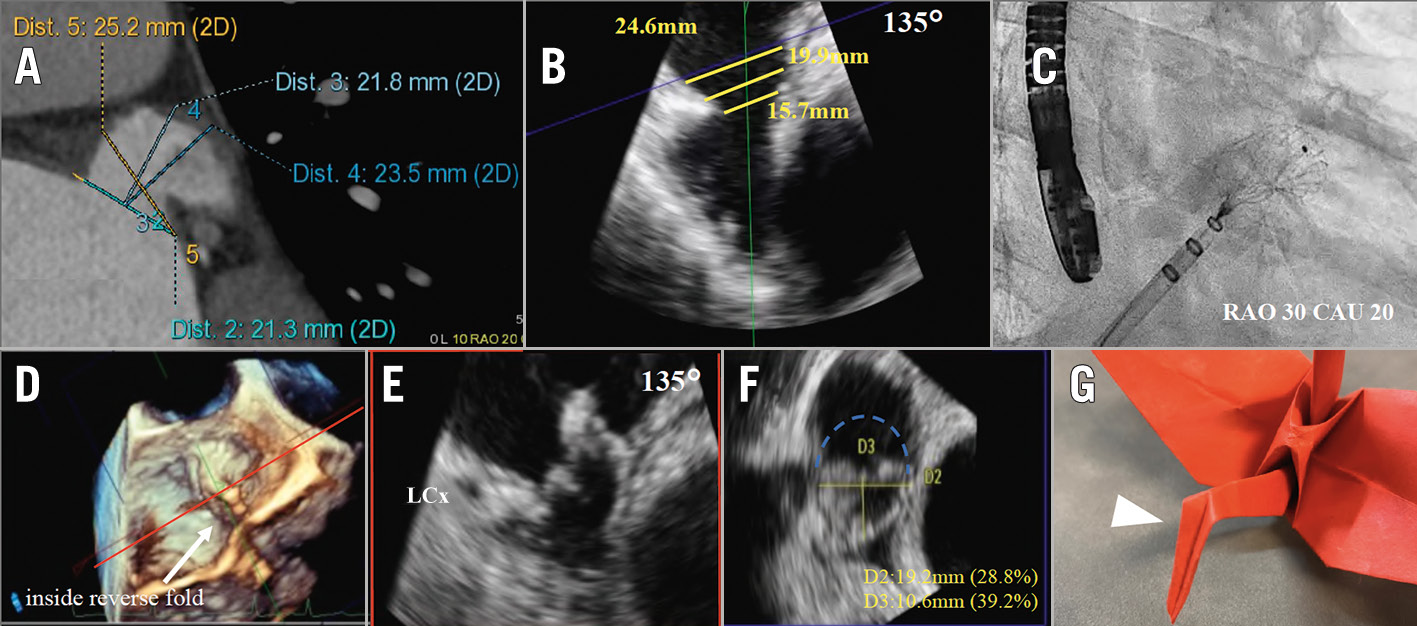
Figure 1. The "origami" shape of a WATCHMAN FLX. A) Preoperative contrast-enhanced CT showed an anterior chicken wing-shaped LAA. B) Intraoperative transoesophageal echography view at 135°. The yellow lines show the landing zone of the left atrial appendage. C) Angiography after the second deployment of the 27 mm device. The device is inadequately expanded, but it is difficult to point out the deformation. D) A three-dimensional multiplanar reconstruction after the second deployment of the 27 mm device. Half of one side of the device’s surface is folded into an inside reverse fold. E) The septal-lateral orientation (red line in D). F) Cross-section horizontal to the device. The dotted line shows the device deformed over half the circumference. G) The inside reverse fold, which is commonly seen when making an origami crane head. 2D: two-dimensional; CAU: caudal; CT: computed tomography; LAA: left atrial appendage; LCx: left circumflex artery; RAO: right anterior oblique
Conflict of interest statement
M. Fukunaga is a proctor for Boston Scientific. The other authors have no conflicts of interest to declare.