Drug-coated balloons (DCBs) represent an emerging technology in interventional cardiology which is gaining more indications in terms of lesion and patient subsets. If drug-eluting stents (DES) remain the preferred and most used technique for revascularisation worldwide1, DCBs are now often considered the first option in indications such as in-stent restenosis (ISR) and de novo lesions in small vessel disease (SVD)2. Several studies have recently been published to test the efficacy and safety of this technology in other clinical and lesion settings3, and the usage of DCBs, eluting either paclitaxel or sirolimus, is further expanding its indications all over the world4. According to the Japanese Association of Cardiovascular Intervention and Therapeutics, East Asian populations are culturally opposed to the long-term implantation of foreign materials, such as stents, into their bodies. This difference in cultural beliefs may result in higher use of the DCB technique compared to other techniques that require permanent implants, impacting clinical outcomes following DCB angioplasty when comparing the East Asian and Caucasian populations5.
The performance of DCBs in various populations can be affected by several physiological and biological factors, which will influence how patients treated with DCBs respond to the treatment and, subsequently, their efficacy and safety outcomes. First, genetic variability can affect drug metabolism and response, and receptor variations can influence the pharmacokinetics and pharmacodynamics of the drugs used in DCBs. Notably, the East Asian population has been found to have a mutation in the CYP2C19 gene, which can affect the metabolism of drugs coated on balloons, such as paclitaxel and sirolimus6. Factors related to vessel physiology, e.g., endothelial function and vascular reactivity, can also vary between populations, leading to different outcomes7. Variations in plaque composition and distribution, and the occurrence of ISR, can also vary between East Asian and Caucasian populations. It is well known that East Asian and Caucasian populations have different diets, and dietary differences affecting lipid profiles and systemic inflammation may alter the local vascular environment and response to DCBs8.
The focus of this study is to determine whether a sirolimus-coated balloon (SCB) is associated with meaningful clinical differences between geographical areas by comparing clinical outcomes between patients enrolled in East Asian and Caucasian centres participating in the EASTBOURNE prospective study.
Methods
Study design and population
The EASTBOURNE Registry (ClinicalTrials.gov: NCT03085823) is a prospective, multicentre, independent, investigator-driven study which enrolled an all-comer population treated with the MagicTouch SCB (Concept Medical) at 38 international centres in Europe and East Asia. The cases enrolled in this study were collected from different regions representing the East Asian and Caucasian populations. By including a diverse range of cases, this study aimed to provide more accurate and comprehensive results that can be applied to a larger population. Eligible patients had coronary artery disease (CAD) with a clinical indication for percutaneous coronary intervention (PCI) with DCBs. Investigators had to demonstrate proficiency by having performed at least 30 DCB angioplasties annually over the previous 5 years.
The inclusion criteria for this study were quite broad, allowing for all clinical indications for PCI with SCBs, as determined by the investigator. However, exclusion criteria were put in place to ensure the safety and effectiveness of the study. These included patients with known hypersensitivity or contraindications to certain medications, as well as target lesions or vessels with specific characteristics, such as severe calcification, high vessel tortuosity or visible thrombus. It is important to note that left main stem disease and ST-segment elevation myocardial infarction (STEMI) did not automatically disqualify a patient from participating in the study. The primary endpoint was target lesion revascularisation (TLR) at 12 months. The secondary endpoints were all-cause death and the occurrence of major adverse cardiovascular events (MACE) during follow-up, defined as a composite of TLR, myocardial infarction (MI), and cardiac death. Procedural success was defined as angiographic success without in-hospital complications. The occurrence of MI during follow-up was also analysed. Follow-up visits were programmed at 30 days, 6 months, and 12 months post-procedure via clinic visits and telephonic surveys. This article specifically reports 12-month outcomes based on ethnic origin.
Main study results
The preliminary and main findings of the EASTBOURNE Registry have been detailed in other publications910. In summary, the study included a total cohort of 2,123 patients, addressing 2,440 lesions. Among the patients, 55% presented with de novo lesions, while 45% had ISR. At 12-month follow-up, which was available for 92.5% of the patients, TLR was observed in 5.9% of lesions, MACE occurred in 9.9% of patients, and the overall rate of all-cause death was 2.5%. Multivariate analysis identified ISR as the primary determinant for the occurrence of the primary endpoint, with an odds ratio of 5.5 (95% confidence interval [CI]: 3.38-8.88). All patients included in this study had clinical follow-ups at 30 days, 6 months and 12 months.
Device description and procedure
The MagicTouch SCB features a nanocarrier technology with a dose of 1.27 micrograms of sirolimus/mm2 of the balloon11. The device is offered in various dimensions, ranging from 10 mm to 40 mm in length and 1.5 mm to 4 mm in diameter, and its characteristics are described elsewhere12.
Proximal and distal references were identified as locations with the largest lumen diameter within a 10 mm segment both proximal and distal to the plaque. The procedure was carried out according to international guidelines or consensus documents13141516. Heparin was administered following sheath insertion, along with loading doses of antiplatelets depending on the patient’s clinical presentation and following investigator judgement. Aspirin was continued indefinitely, and the second antiplatelet drug was prescribed for up to 1 month post-procedure in the absence of additional stenting, or for 6-12 months in cases of DES implantation or presentation with acute coronary syndrome. The DCB was inflated to its nominal pressure and maintained for a minimum of 30 seconds. The DCB diameter was adjusted to the reference vessel diameter, maintaining a balloon-to-vessel ratio of 0.8-1.0/1.0, while the balloon length was selected to exceed both lesion ends by at least 3 mm. The decision to place a stent post-DCB angioplasty in a bailout fashion was at the discretion of the operator and was suggested in cases of coronary dissection of type >B or impaired coronary flow. The protocol also recommended against stenting small and uncomplicated dissections of type A or B.
Statistical analysis
The distribution of continuous variables was assessed using the Shapiro-Wilk test. Continuous variables are reported as means with standard deviations or medians with interquartile ranges (IQR) in case of Gaussian or non-Gaussian distribution, respectively. Comparisons between two groups used the Student’s t-test or Mann-Whitney U test, as appropriate. Comparisons of continuous variables among more than two groups were performed using analysis of variance (ANOVA). Categorical variables are reported as frequencies and percentages and were compared by the chi-square test or Fisher’s exact test, as appropriate. To control for the effect of potential confounding factors, one-to-one propensity score matching (PSM) was performed using the nearest-neighbour method without replacement, with a calliper width within 0.2 times the pooled standard deviation of the logit of the propensity scores. A Cox survival analysis was conducted for the endpoint all-cause death, with stratification by country, and reported as Kaplan-Meier curves. All p-values were based on two-sided tests. A p-value less than 0.05 was considered statistically significant for all the study analyses. The analyses were performed using R version 4.0.5 (R Foundation for Statistical Computing), equipped with the packages “MatchIt”, “survival”, “survminer”, and “Rcpp”. The variables used for propensity score matching were selected based on their association with the probability of being in one group or the other, as well as their significant imbalance in the unadjusted population. These variables included age, diabetes, smoking status, dyslipidaemia, body mass index, family history of CAD, prior MI, peripheral artery disease, left ventricular ejection fraction, haemoglobin levels, angina, lesion length, right ventricular dysfunction, and whether the procedure was de novo or in-stent restenosis. For procedural characteristics, only selected variables were added to maintain a parsimonious model and avoid excessively reducing the number of matched pairs.
Results
Between September 2016 and December 2020, a total of 2,084 patients were included in the Caucasian versus East Asian ethnicity-based post hoc study of EASTBOURNE. Overall, a total of 1,657 patients were enrolled in the Caucasian subgroup and 427 patients in the East Asian subgroup.
Baseline characteristics
Baseline characteristics are reported in Supplementary Table 1. The average age was 67 years, 81.2% were male, and 41.6% had diabetes. Multivessel coronary artery disease (MV-CAD) was present in 59.4% of the patients, previous MI in 42.9%, and previous PCI in 66.2%. The baseline characteristics were significantly different between groups. In the Caucasian group, patients were older with a lower incidence of diabetes (38.7% vs 52.9%; p<0.001) but more frequent family history of coronary disease (26% vs 11%; p<0.001), as well as higher rates of previous PCI (73.4% vs 38.4%; p<0.001) and previous coronary artery bypass grafting (CABG; 13.5% vs 4.7%; p<0.001). However, the lower diabetes incidence, which is not influenced by ethnicity, may not have significantly impacted the outcomes of the study. Stable angina pectoris was the most common disease type in both groups.
After propensity matching (n=602 patients), there were no significant differences in the baseline characteristics between the groups apart from greater STEMI rates in the Caucasian group compared to East Asian patients (8.7% vs 4.3%) (Table 1). However, significant differences regarding antiplatelet regimens persisted after propensity matching (Table 1).
Table 1. Baseline characteristics of patients after propensity matching.
| Characteristic | Overalln=602 | Caucasiann=301 | East Asiann=301 | p-value |
|---|---|---|---|---|
| Age, years | 62.00 [55.00, 69.00] | 62.00 [55.00, 70.00] | 62.00 [55.00, 69.00] | 0.560 |
| Male sex | 498 (82.7) | 245 (81.4) | 253 (84.1) | 0.451 |
| BMI, kg/m² | 26.02 [23.54, 29.28] | 26.12 [24.07, 28.93] | 25.71 [23.39, 29.41] | 0.392 |
| Diabetes | 306 (50.8) | 161 (53.5) | 145 (48.2) | 0.221 |
| Hypercholesterolaemia | 443 (73.6) | 222 (73.8) | 221 (73.4) | 1.000 |
| Smoker | 132 (21.9) | 63 (20.9) | 69 (22.9) | 0.622 |
| Renal insufficiency | 60 (10.0) | 31 (10.3) | 29 (9.6) | 0.892 |
| Family history of CAD | 90 (15.0) | 47 (15.6) | 43 (14.3) | 0.732 |
| Stroke | 25 (4.2) | 15 (5.0) | 10 (3.3) | 0.414 |
| Congestive heart failure | 43 (7.1) | 17 (5.6) | 26 (8.6) | 0.205 |
| Previous myocardial infarction | 202 (33.6) | 104 (34.6) | 98 (32.6) | 0.666 |
| Previous CABG | 41 (6.8) | 25 (8.3) | 16 (5.3) | 0.195 |
| Previous PCI | 304 (50.5) | 177 (58.8) | 127 (42.2) | <0.001 |
| Peripheral artery disease | 306 (50.8) | 161 (53.5) | 145 (48.2) | 0.221 |
| MV-CAD | 339 (56.3) | 178 (59.1) | 161 (53.5) | 0.189 |
| LVEF, % | 55.00 [50.00, 60.00] | 55.00 [50.00, 60.00] | 55.00 [50.00, 60.00] | 0.138 |
| Creatinine, mg/dL | 0.98 [0.84, 1.16] | 0.98 [0.80, 1.19] | 0.98 [0.85, 1.14] | 0.805 |
| Haemoglobin, g/dL | 13.60 [12.43, 14.90] | 13.50 [12.50, 14.80] | 13.90 [12.30, 15.00] | 0.408 |
| Clinical indication for PCI | 0.984 | |||
| Non-STEMI | 77 (12.8) | 40 (13.3) | 37 (12.3) | |
| Silent ischaemia | 96 (15.9) | 46 (15.3) | 50 (16.6) | |
| Stable angina | 265 (44.0) | 133 (44.2) | 132 (43.9) | |
| STEMI | 54 (9.0) | 26 (8.7) | 13 (4.3) | |
| Unstable angina | 110 (18.3) | 56 (18.6) | 54 (17.9) | |
| Data are presented as median [IQR] or n (%). BMI: body mass index; CABG: coronary artery bypass grafting; CAD: coronary artery disease; IQR: interquartile range; LVEF: left ventricular ejection fraction; MV-CAD: multivessel coronary artery disease; PCI: percutaneous coronary intervention; STEMI: ST-segment elevation myocardial infarction | ||||
Procedural characteristics
In terms of procedural characteristics of the 2,318 lesions treated, the reference vessel diameter was 2.5 (IQR 2.10, 3.00) mm, and the length of the lesion was 16.66 (IQR 12.00, 23.00) mm. There was no difference in the number of lesions treated per patient. Specifically, over 80% of both groups had small CAD (<2.75 mm, 88.4% in Caucasians vs 91.3% in East Asians; p=0.061), and over 40% underwent multivessel PCI (41.9% vs 42.2%; p=0.956).
The procedural characteristics per lesion were significantly different between the two groups, as described in Supplementary Table 2. The rate of de novo lesions (87.2% vs 47.5%; p<0.001) was higher in East Asians. On the other hand, the rate of in-stent restenosis (52.5% vs 12.8%; p<0.001) was higher in the Caucasian population. Bailout stenting after DCB use occurred more frequently in the Caucasian population (9.2% vs 1.9%; p<0.001). In contrast, the rate of final dissections was higher in the East Asian population (6.6% vs 2.8%; p=0.001). Conversely, reference vessel diameter was similar in both groups (2.50 [IQR 2.25, 3.00] mm vs 2.50 [IQR 2.00, 2.75] mm; p<0.001). The lesion length was longer in East Asians compared to Caucasians (20.00 [IQR 13.59, 25.00] mm vs 18.59 [IQR 15.00, 25.00] mm; p=0.970). Procedural success was achieved in over 95% of both groups (97.9% vs 96.8%; p=0.169).
After adjustment of variables by propensity matching, out of 669 lesions treated with DCBs, in the Caucasian population, we found a lower predilatation rate and shorter DCBs used at higher pressures; Caucasian patients were also treated with a higher rate of bailout stenting. All other technical characteristics and in-hospital outcomes were not significantly different (Table 2).
Table 2. Procedural characteristics (after PSM).
| Per patient | Overalln=602 | Caucasiann=301 | East Asiann=301 | p-value |
|---|---|---|---|---|
| Vascular approach | 0.285 | |||
| Femoral | 121 (20.1) | 56 (18.6) | 65 (21.6) | |
| Radial | 479 (79.6) | 243 (80.7) | 236 (78.4) | |
| Multivessel PCI | 241 (40.0) | 121 (40.2) | 120 (39.9) | 1.000 |
| Contrast media use, mL | 160.00 [120.00, 200.00] | 180.00 [120.00, 257.50] | 150.00 [100.00, 180.00] | <0.001 |
| Fluoroscopy time, minutes | 19.00 [12.50, 34.00] | 20.00 [13.00, 34.00] | 18.00 [11.25, 32.75] | 0.115 |
| Per lesion | Overalln=669 | Caucasiann=336 | East Asiann=333 | p-value |
| Percentage diameter stenosis, % | 80.00 [74.00, 90.00] | 85.25 [80.00, 90.00] | 80.00 [70.00, 90.00] | 0.007 |
| RVD, mm | 2.50 [2.00, 2.75] | 2.50 [2.00, 2.70] | 2.50 [2.00, 2.75] | 0.990 |
| Lesion length, mm | 20.00 [14.78, 25.00] | 18.59 [15.00, 25.00] | 20.00 [13.59, 25.00] | 0.970 |
| De novo lesions | 536 (80.1) | 263 (78.3) | 273 (82.0) | 0.246 |
| ISR | 132 (19.7) | 74 (22.0) | 58 (17.4) | 0.146 |
| Lesion type | 0.291 | |||
| A | 126 (18.8) | 55 (16.4) | 71 (21.3) | |
| B1 | 243 (36.3) | 121 (36.0) | 122 (36.6) | |
| B2 | 157 (23.5) | 81 (24.1) | 76 (22.8) | |
| C | 143 (21.4) | 79 (23.5) | 64 (19.2) | |
| Predilatation | 621 (92.8) | 294 (87.5) | 327 (98.2) | <0.001 |
| Predilatation balloon length, mm | 15.00 [12.00, 20.00] | 15.00 [12.00, 20.00] | 15.00 [13.00, 15.00] | 0.081 |
| Predilatation balloon diameter, mm | 2.00 [2.00, 2.50] | 2.00 [2.00, 2.50] | 2.25 [2.00, 2.50] | 0.005 |
| DCB length, mm | 20.00 [20.00, 30.00] | 20.00 [15.00, 30.00] | 25.00 [20.00, 30.00] | <0.001 |
| DCB diameter, mm | 2.50 [2.00, 2.75] | 2.50 [2.00, 2.75] | 2.50 [2.00, 2.75] | 0.319 |
| DCB inflation pressure, atm | 8.00 [6.00, 12.00] | 10.00 [8.00, 12.00] | 7.00 [6.00, 10.00] | <0.001 |
| Procedural complications | 13 (1.9) | 7 (2.1) | 6 (1.8) | 1.000 |
| Bailout stenting | 55 (8.2) | 46 (13.7) | 9 (2.7) | <0.001 |
| Final TIMI 3 flow | 648 (96.8) | 328 (97.6) | 320 (96.1) | 0.535 |
| Postprocedural dissection remaining | 95 (14.2) | 45 (13.4) | 50 (15) | 0.293 |
| Angiographic success | 652 (97.5) | 327 (97.3) | 325 (97.6) | 1.000 |
| Procedural success | 643 (96.1) | 320 (95.2) | 323 (97.0) | 0.317 |
| Data are presented as median [IQR] or n (%). DCB: drug-coated balloon; ISR: in-stent restenosis; PCI: percutaneous coronary intervention; PSM: propensity score matching; RVD: reference vessel diameter; TIMI: Thrombolysis in Myocardial Infarction | ||||
Clinical outcomes
Clinical outcomes were available for 92.5% of the patients at a median follow-up of 366.5 (IQR 364, 388) days and showed significant differences among the groups (Supplementary Table 3). After adjustment for confounding factors (n=602 patients), the incidence of the primary endpoint, TLR, was higher in Caucasians versus East Asians, (6.0% vs 1.5%; p<0.001), whereas neither all-cause death (including cardiac and non-cardiac death) nor spontaneous MI differed significantly. The rate of MACE (defined as the composite of TLR, MI and cardiac death) was significantly higher in the Caucasian population (10.6% vs 3.7%; p=0.001). Interestingly, the occurrence of Bleeding Academic Research Consortium (BARC) 2-5 bleeding was lower in Caucasians as compared to East Asians (0.0% vs 5.0%; p<0.001) (Figure 1, Table 3). The difference in antiplatelet therapy, specifically aspirin and clopidogrel, between the East Asian and Caucasian populations may explain the higher incidence of bleeding events in the East Asian population even after matching. Aspirin usage was significantly higher in East Asians (94.7%) compared to Caucasians (70.8%; p<0.001), while clopidogrel usage was 42.9% in East Asians compared to 22.6% in Caucasians (p<0.001) (Table 4).
Figure 2 shows the Kaplan-Meier curve of incidence of all-cause death. In addition, the statistical analysis shows that there is an adjusted hazard ratio for death of 2.77 before the use of propensity score matching, with a 95% CI of 0.15-53.05. After implementing PSM, the adjusted hazard ratio drops to 1.23 with a 95% CI of 0.16-9.53.
Our analysis also shows a similar outcome regarding the primary and secondary endpoints after stratification by treated lesion type, de novo vs ISR (Figure 3).
According to the love plot, significant standardised mean differences were observed in the unadjusted cohort, but these differences were well balanced after PSM was applied (Figure 4). The data were also balanced after PSM, as shown in Figure 4. This indicates that the matching process was successful in creating a more balanced and comparable cohort for analysis.
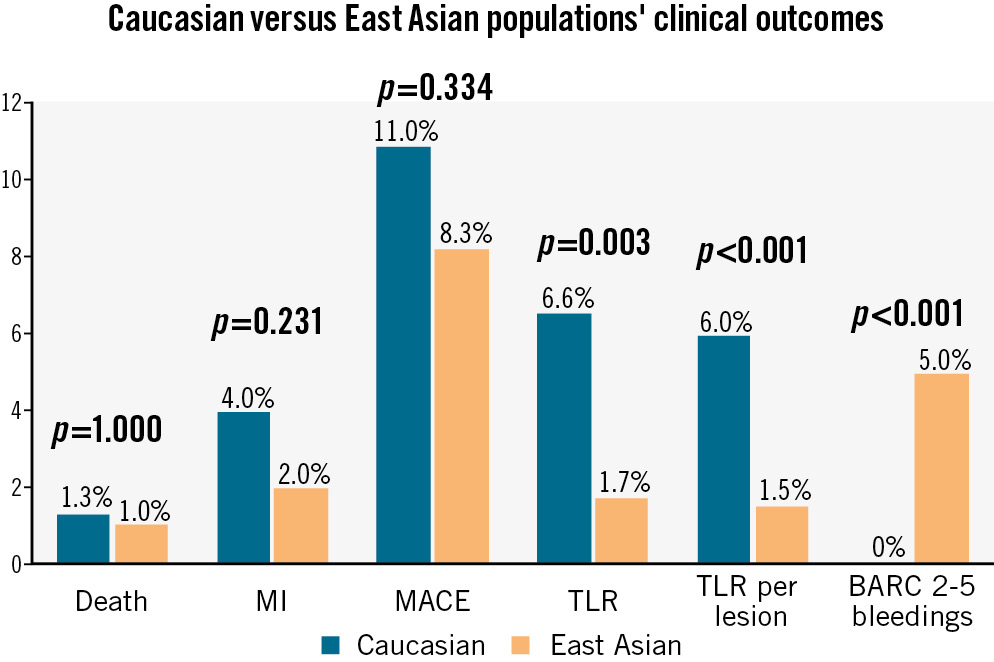
Figure 1. Caucasian and East Asian clinical outcomes (PSM population). BARC: Bleeding Academic Research Consortium; MACE: major adverse cardiovascular events; MI: myocardial infarction; PSM: propensity score-matched; TLR: target lesion revascularisation
Table 3. Clinical outcomes after propensity score matching.
| Outcome | Overalln=602 | Caucasiann=301 | East Asiann=301 | p-value |
|---|---|---|---|---|
| All-cause death (including cardiac and non-cardiac death) | 7 (1.2) | 4 (1.3) | 3 (1.0) | 1.000 |
| MI | 18 (3.0) | 12 (4.0) | 6 (2.0) | 0.231 |
| MACE (composite of TLR, MI and cardiac death) | 58 (9.6) | 33 (11.0) | 25 (8.3) | 0.334 |
| TLR (per lesion) | 25 (4.2) | 20 (6.0) | 5 (1.5) | <0.001 |
| BARC 2-5 bleeding | 15 (2.5) | 0 (0) | 15 (5.0) | <0.001 |
| Values are n (%). BARC: Bleeding Academic Research Consortium; MACE: major adverse cardiovascular events; MI: myocardial infarction; TLR: target lesion revascularisation | ||||
Table 4. Antiplatelet agents after propensity score matching.
| Antiplatelet agent used at 1-year follow-up | Overalln=602 | Caucasiann=301 | East Asiann=301 | p-value |
|---|---|---|---|---|
| Aspirin | 498 (82.7) | 213 (70.8) | 285 (94.7) | <0.001 |
| Clopidogrel | 197 (32.7) | 68 (22.6) | 129 (42.9) | <0.001 |
| Prasugrel | 8 (1.3) | 8 (2.7) | 0 (0) | 0.007 |
| Ticagrelor | 144 (23.9) | 35 (11.6) | 109 (36.2) | <0.001 |
| Values are n (%). | ||||
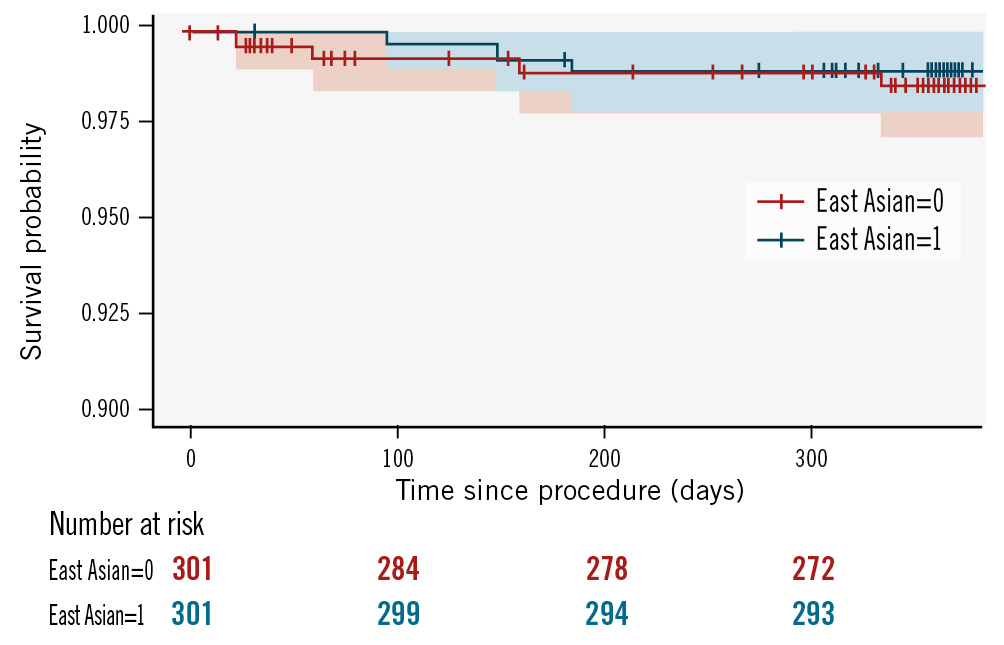
Figure 2. Kaplan-Meier curves for the occurrence of all-cause death (propensity score-matched population).
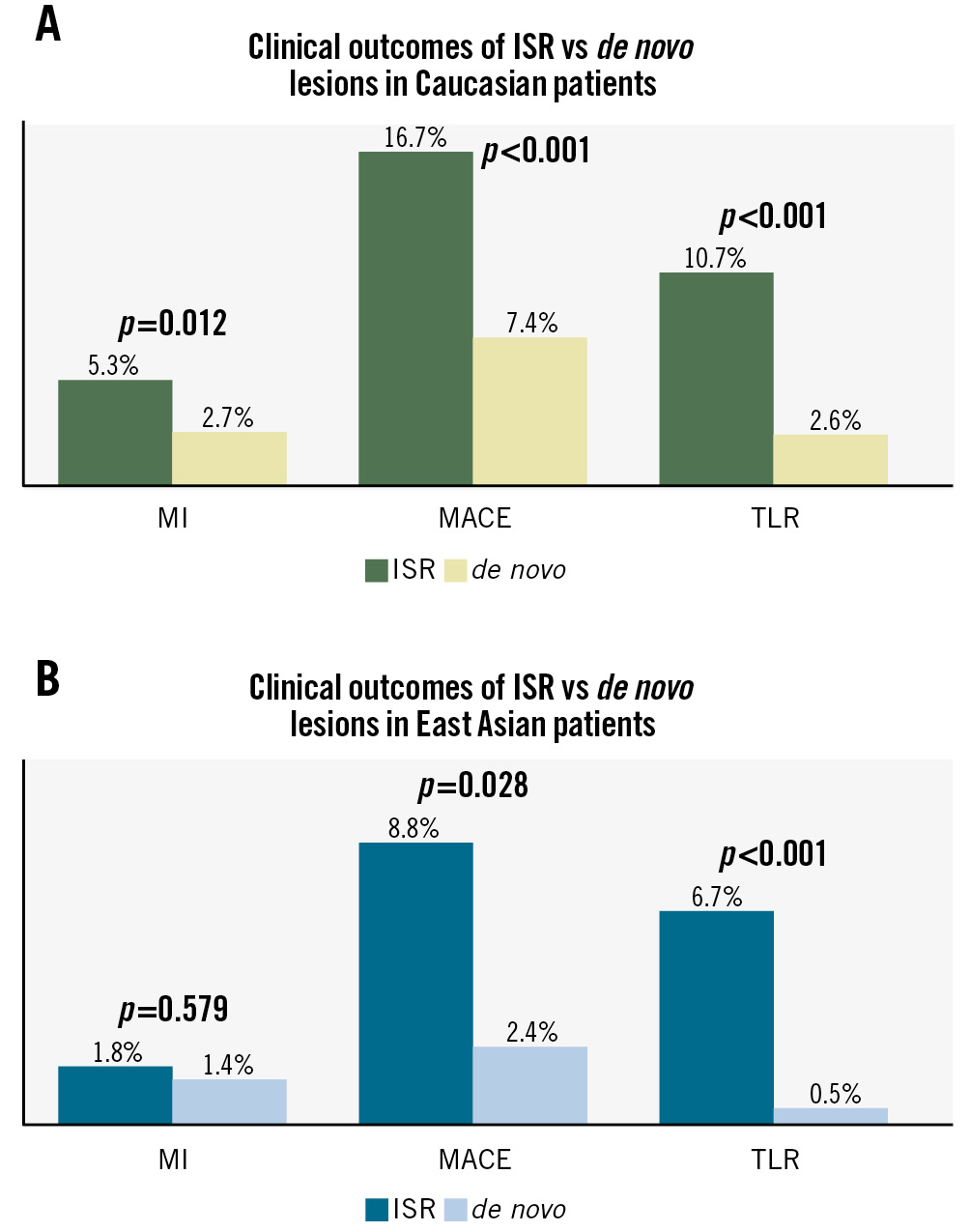
Figure 3. Clinical outcomes based on lesion type (ISR and de novo). ISR: in-stent restenosis; MACE: major adverse cardiovascular events; MI: myocardial infarction; TLR: target lesion revascularisation
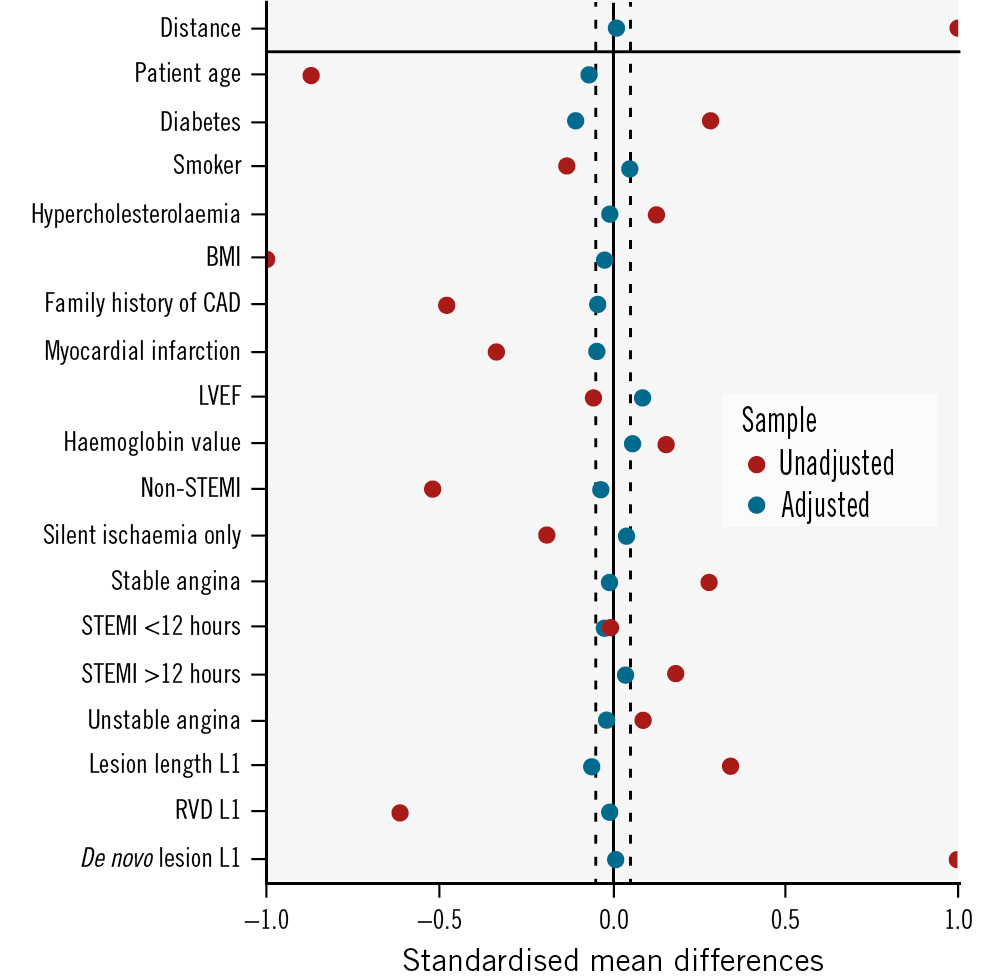
Figure 4. Love plot showing covariate balance before and after propensity score matching. BMI: body mass index; CAD: coronary artery disease; LVEF: left ventricular ejection fraction; RVD: reference vessel diameter; STEMI: ST-segment elevation myocardial infarction
Discussion
In this large-scale prospective study, SCBs used in a diverse CAD population with a broad spectrum of clinical indications showed the following (Central illustration):
• The clinical outcome after SCB PCI was worse in the Caucasian population in terms of TLR.
• BARC 2-5 bleeding was more frequent in the East Asian population.
• SCB performance seems to be reduced in ISR lesions as compared to de novo lesions in both populations, with a similar difference observed.
Caucasians were found to have more severe disease, more in-stent restenosis, less predilatation, and required more bailout stenting. On the other hand, East Asians had higher rates of dual antiplatelet therapy and better lesion preparation. These important differences in factors could potentially explain the higher rates of TLR observed in the study.
At present, few studies have analysed the clinical and procedural differences between Caucasian and Asian populations with CAD or undergoing coronary angioplasty, and most of these studies investigated either Caucasian or Asian populations alone. In addition, no published study describes the outcomes between patients of different geographical areas treated with DCBs so far.
Geographical differences in patients with acute myocardial infarction were studied in the PARADISE-MI trial, which included 23% of patients from Eastern Europe, 18% of patients from Western Europe, 12% of patients from Southern Europe, 10% from Northern Europe, 12% from Latin America, 9% from North America, 10% from East and Southeast Asia, and 6% from South Asia. This study found that patients treated in Asia were younger compared to other geographical areas and had different comorbidities with higher rates of diabetes and atrial fibrillation. Patients from Asia had higher rates of STEMI and a lower rate of primary percutaneous coronary intervention17. Additionally, the usage of angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, and beta blockers was lower in Asian patients compared to other patients from other global regions. In terms of outcome, the incidence of death or heart failure post-MI was lowest in South Asia, at a rate of 4.6%, and highest in Latin America, at a rate of 9.2%. In conclusion, PARADISE-MI confirmed that there were substantial differences between patients with MI from different regions regarding baseline characteristics, treatment approach, and outcomes, and it also gave us some insights to consider regional variations when treating patients with myocardial infarction using either drug-eluting stents, DCBs, or CABG but unfortunately did not go into the details of each category17.
Another study that compared East Asians and Europeans, by Kwon et al18, reported that intravascular ultrasound- or optical coherence tomography-guided interventions were more commonly used in East Asian patients due to specific reimbursement regulations, which might have contributed to better clinical outcomes despite the shorter duration of dual antiplatelet therapy18.
The EPICOR and EPICOR ASIA trials19 were two large studies comparing global geographical variations in STEMI management and post-discharge mortality that included 4,943 patients from Europe and Latin America and 6,616 from Asia. Use of reperfusion therapy was lowest in India, with a rate of 54%, and highest in Southern Europe, with a rate of 81%. Primary PCI was least used in India and most commonly used in Northern Europe as the primary therapeutic approach, with a rate of 65.6%. Fibrinolysis was less commonly used in China, with a rate of 8.1%, and most commonly used in Southeast Asia, with a rate of 34.2%. Time to primary PCI was lowest in Northern Europe, and mortality rates were lowest in Northern Europe up to two years after the MI event19.
Several studies have analysed the performance of DCBs in European, Chinese, or Malaysian patients. The PICCOLETO II trial compared the performance of a paclitaxel DCB with an everolimus DES in European patients with de novo lesions in small coronary arteries and found that DCB performance was superior to the stent in terms of late lumen loss at 6 months20; an improved clinical outcome was also found after 3 years21. BASKET-SMALL2 enrolled patients with a reference vessel diameter <3 mm at 14 hospitals in Germany, Switzerland, and Austria. The 758 patients treated showed the non-inferiority of DCBs as compared to DES in terms of MACE up to 3 years22. The RESTORE SVD trial enrolled a Chinese population with SVD and showed similar angiographic performance between paclitaxel DCBs and DES at 9 months, along with a similar clinical outcome at 5 years2324. Caucasian and East Asian patients with small vessel disease enrolled in these trials were treated with paclitaxel DCBs, which showed non-inferiority to DES at different follow-up durations.
The clinical differences depicted in this EASTBOURNE subanalysis can be attributed to several factors. The Caucasian population enrolled in EASTBOURNE had a higher initial percentage diameter stenosis and had lower rates of lesion predilatation (87% vs 98%; p<0.001), despite this being strongly recommended in the study protocol. Previous literature data show the importance of adequate lesion preparation before drug delivery via DCB, and any tool can be used to achieve this goal25; the clinical outcome of DCB therapy is in fact impaired when lesion predilatation is adequately performed or is ineffective26. Moreover, despite propensity matching adjustment, the Caucasian population underwent a higher rate of bailout stenting as compared to the East Asian one (13.7% vs 2.7%; p<0.001); stenting after treatment with DCBs has been associated with impaired outcomes and the need for TLR in other studies22.
Racial differences may also play a role in terms of bleeding risk clinical outcomes and performance after DCB angioplasty. East Asian populations are prone to display higher rates of bleeding compared to their European counterpart27, as previous literature has highlighted, a phenomenon known as the “East Asian Paradox”28. Genetic factors, such as polymorphisms in drug-metabolising enzymes like CYP2C19, are more common in East Asians and can affect drug response and bleeding risk18. Additionally, differences in platelet reactivity and endothelial function contribute to their unique risk profiles2930. Even with advanced treatments like DCB therapy, these intrinsic factors continue to impact bleeding risk. Furthermore, variations in diet, lifestyle, and comorbid conditions like hypertension and diabetes may also play a role in this persistent tendency3132. However, further studies are required to fully understand and confirm the impact of ethnic factors on clinical outcomes. While some research has shown a correlation between ethnicity and certain health conditions, more extensive and thorough studies are needed to establish a definitive relationship. The higher bleeding risk in East Asian patients in our study could also be partially attributed to the fact that these patients had more usage of the second antiplatelet drug (mostly ticagrelor) in their discharge medications and during clinical follow-up at 1 year compared to Caucasian patients (36.5% vs 9.7%; p<0.001) (Table 4). Another important point to underline is that most of the literature data from DCB studies conducted in Asia or Europe involved patients treated with paclitaxel DCBs, whereas our study exclusively enrolled patients treated with sirolimus DCBs. Few studies have been performed that combined Caucasian and East Asian patients, and, to our knowledge, no study has assessed the difference between these two groups of patients. Understanding these factors can help improve treatment strategies for East Asian patients.
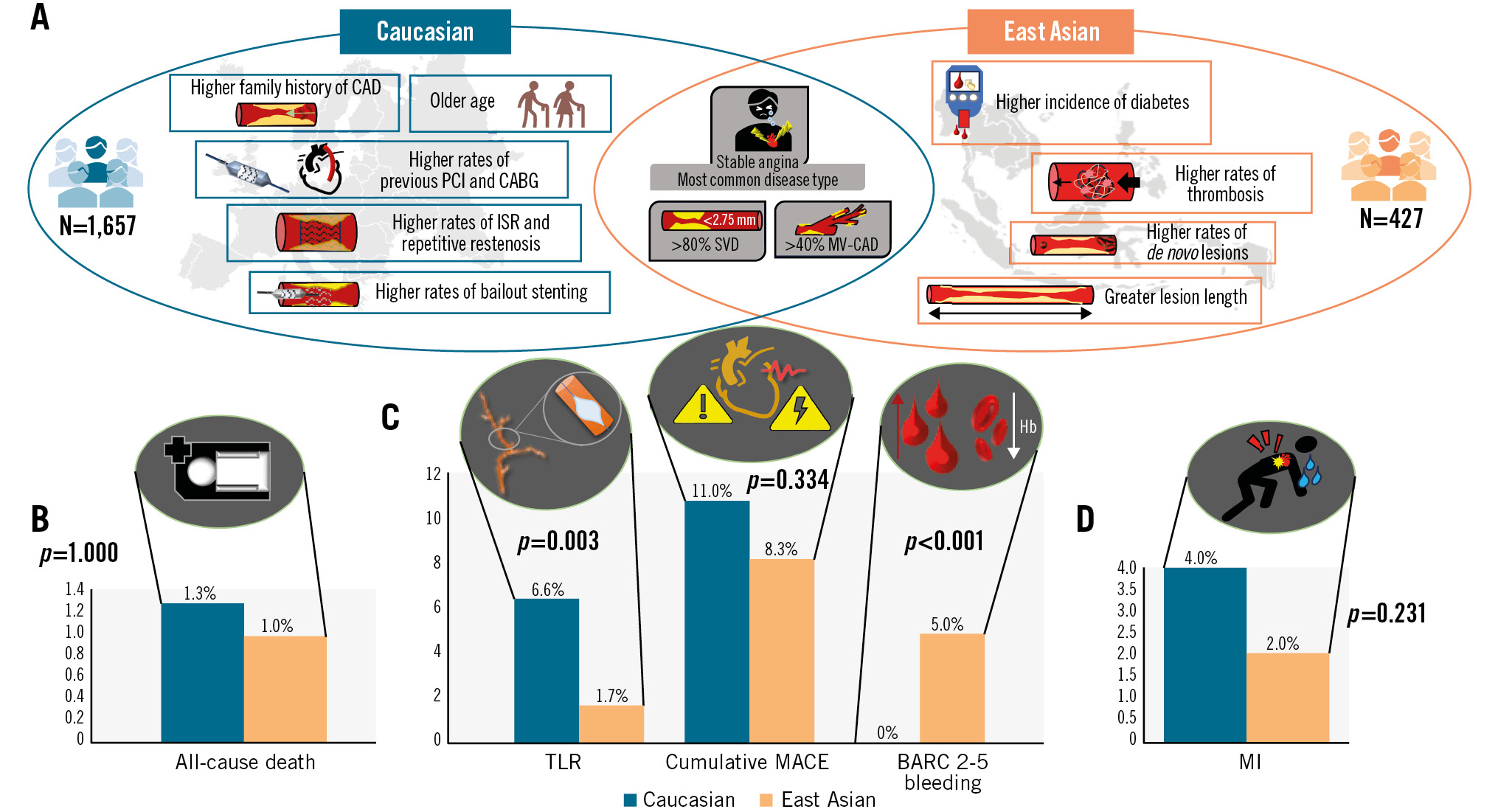
Central illustration. Clinical differences between Caucasian and East Asian patient populations. A) Comparison of baseline characteristics; comparison of clinical outcomes for all-cause death (B); TLR, cumulative MACE, and BARC 2-5 bleeding (C); and MI (D). BARC: Bleeding Academic Research Consortium; CABG: coronary artery bypass grafting; CAD: coronary artery disease; Hb: haemoglobin; ISR: in-stent restenosis; MACE: major adverse cardiovascular events; MI: myocardial infarction; MV-CAD: multivessel coronary artery disease; PCI: percutaneous coronary intervention; SVD: small vessel disease; TLR: target lesion revascularisation
Table 4. Antiplatelet agents after propensity score matching.
| Antiplatelet agent used at 1-year follow-up | Overalln=602 | Caucasiann=301 | East Asiann=301 | p-value |
|---|---|---|---|---|
| Aspirin | 498 (82.7) | 213 (70.8) | 285 (94.7) | <0.001 |
| Clopidogrel | 197 (32.7) | 68 (22.6) | 129 (42.9) | <0.001 |
| Prasugrel | 8 (1.3) | 8 (2.7) | 0 (0) | 0.007 |
| Ticagrelor | 144 (23.9) | 35 (11.6) | 109 (36.2) | <0.001 |
| Values are n (%). | ||||
Limitations
This study included a large number of patients from different geographical areas and different hospitals, with varying experience in DCB usage. Despite adjusting for measured confounding factors using propensity score matching, the different outcomes observed could be a consequence of varying expertise or local practice. Another limitation of this study is the absence of a core lab for assessing the different angiographic parameters during the index PCI. Finally, this is an observational study, and despite prospective patient enrolment, a direct comparison between devices was not performed, and the decision about treatment options was left to the physician’s discretion.
Conclusions
DCB use is increasing in East Asian and Caucasian countries, for both ISR lesions and de novo coronary lesions. The current post hoc analysis of the EASTBOURNE Registry highlights some important clinical differences between Caucasian and East Asian patients treated with SCBs. Further ad hoc and adequately powered studies are needed to determine if the technical differences result in different outcomes.
Impact on daily practice
Clinical and procedural differences between Caucasian and East Asian populations undergoing coronary angioplasty with drug-coated balloons can significantly impact their cardiovascular outcomes. It is important to understand these differences to address disparities. By studying and acknowledging these differences, physicians can develop more personalised and effective treatment plans for their patients, leading to better overall outcomes.
Conflict of interest statement
B. Cortese serves on the advisory board of Concept Medical. The other authors have no conflicts of interest to declare.

