Introduction
Drug-eluting stents (DES) have revolutionised interventional cardiology and have long been established as the standard treatment for percutaneous coronary intervention (PCI). However, concerns remain regarding late adverse events, such as late or very late in-stent restenosis (ISR), even with the new generation of DES. Stent length, stent diameter and overlapping stents are known to be independent predictors of ISR and stent thrombosis123.
The use of drug-coated balloons (DCBs) has been gaining acceptance with the concept of “leave nothing behind”4. The safety and efficacy of DCBs in de novo small and diffuse lesions have been recently shown to be non-inferior to DES5. Their benefits are also proven in de novo lesions in diabetic and high bleeding risk patients6.
The option of a hybrid strategy combining a DES and DCB has been gaining increasing acceptance among interventional cardiologists. This strategy is often adopted in complex PCI involving long diffuse lesions or bifurcation lesions. Data regarding clinical outcomes for this practice are still very limited especially among the Southeast Asian population.
The aim of this study is to assess the safety and clinical outcome of the hybrid strategy (DES and DCB) in the treatment of de novo coronary artery disease. The primary endpoint was target lesion failure (TLF) in the DES/DCB-treated segment at 12 months. TLF is defined as the composite of cardiac death, target vessel myocardial infarction (TVMI) and ischaemia-driven target lesion revascularisation (ID-TLR) in the DES- and/or DCB-treated segment. The secondary endpoint was all-cause mortality, major adverse cardiovascular events (MACE) and TLF predischarge or within 30 days of the procedure. MACE included acute myocardial infarction, stroke and cardiac death. TLF is defined as the composite of cardiac death, TVMI (excluding periprocedural myocardial infarction) and ID-TLR in the DES- and/or DCB-treated segment.
Methods
Study design
This is a retrospective, single-centre, observational study of patients who were admitted to the National Heart Institute (IJN), Kuala Lumpur from 1 July 2021 to 30 June 2022 (12 months) for chronic or acute coronary syndrome (ACS). All patients who underwent PCI treatment were screened. Patients who were treated using a hybrid strategy of DES and DCB for de novo coronary artery disease were enrolled in the study.
Exclusion criteria were as follows:
1. Patients aged 18 and below.
2. Patients whose PCI was done to treat a segment with ISR.
In our study, the hybrid strategy is defined as a slight overlap of a new-generation DES (usually larger in diameter and located proximally) and a DCB (usually smaller in diameter and located distally) in a single coronary vessel. Bifurcation lesions that were treated with the hybrid strategy, i.e., the main branch was treated with a DES and the side branch was treated with a DCB, were also enrolled in the study.
The recruited subjects were followed up for a year after PCI. Patients lost to follow-up were excluded from the outcome analysis. The study was reviewed by the Clinical Research Department of the Institut Jantung Negara (National Heart Institute) and was approved by the ethics department.
Data collection and statistics
Patients’ clinical data were collected from a registry database, patient medical records, electronic medical information system and phone calls. All clinic visits and hospital admissions were reviewed. The indication for PCI was recorded and analysed. All statistics are descriptive. Categorical variables are presented as percentages. Continuous data are presented as mean±standard deviation (SD).
Drug therapy
All patients undergoing PCI were pretreated with a loading dose of dual antiplatelet therapy (DAPT). This consisted of a loading dose of aspirin 300 mg in combination with a P2Y12 inhibitor (clopidogrel 300 mg or ticagrelor 180 mg) for patients who were antiplatelet naïve. Patients who were already on these medications continued with their regular doses.
Following the procedure, patients were prescribed 12 months of DAPT with the exception of patients in the high bleeding risk group. In such cases, the duration of DAPT was permitted to be reduced based on the clinical judgement of the treating physician7. Additionally, all study patients received standard medical therapy post-procedure including statins, beta blockers and angiotensin receptor blockers.
PCI procedure
Diagnostic angiography evaluation
All patients who underwent diagnostic coronary angiography were evaluated for coronary artery disease. If PCI was indicated, the decision for treatment with DES only, DCB only or the hybrid strategy was made at the discretion of the operator.
Lesion preparation
Optimal lesion preparation is mandatory for all PCIs. The balloons used included semicompliant, non-compliant and scoring balloons. Intracoronary imaging modalities such as intravascular ultrasound (IVUS) and intracoronary optical coherence tomography (OCT) were employed for further vessel evaluation at the operator’s discretion. Additionally, atherectomy techniques, such as rotablation, orbital atherectomy, or intracoronary lithotripsy, were utilised for heavily calcified lesions.
For segments treated with a DCB, vessel preparation adhered to current international recommendations, with a balloon-to-vessel ratio of 0.8-1.0. Following predilation, the DCB segment was assessed, and if residual diameter stenosis was ≤30% and Thrombolysis in Myocardial Infarction (TIMI) 3 flow without flow-limiting dissection was achieved, DCB application ensued6. The inflation time for the DCB was set at 30-60 seconds, with a preference for 60 seconds, unless the patient experienced angina or haemodynamic instability due to prolonged ischaemia.
Drug-eluting stents and drug-coated balloons
The selection of the type of new-generation DES and DCB was left to the discretion of the operator. The specific DES and DCBs utilised in our study are listed below:
Drug-eluting stents
Everolimus-eluting stents: SYNERGY (Boston Scientific); SYNERGY MEGATRON (Boston Scientific); XIENCE Expedition (Abbott); XIENCE Alpine (Abbott); XIENCE Sierra (Abbott)
Sirolimus-eluting stents: COMBO Plus (OrbusNeich); Cre8 EVO (Alvimedica); Orsiro (Biotronik); Ultimaster (Terumo); Ultimaster Tansei (Terumo)
Zotarolimus-eluting stents: Resolute Onyx (Medtronic)
Biolimus-eluting stents: BioFreedom (Biosensors); BioFreedom Ultra (Biosensors)
Drug-coated balloons
Paclitaxel-coated balloons: AGENT (Boston Scientific); RESTORE (Cardionovum); SeQuent Please NEO (B. Braun); Panthera Lux (Biotronik)
Sirolimus-coated balloons: MagicTouch (Concept Medical); SELUTION SLR (MedAlliance)
Post-dilation
Stented segments were postdilated with non-compliant balloons for optimal approximation of the stent.
Bifurcation percutaneous coronary intervention
For bifurcation lesion PCIs, DCBs were designated to address the side branch (SB), while DES were used for the main vessel (MV) and main branch (MB). Following the separate advancement of guidewires into both branches, adequate predilation was performed on each segment before the introduction of the DES and DCB.
After adequate predilation, the SB segment was assessed for residual diameter stenosis ≤30% and TIMI 3 flow without flow-limiting dissection. If these criteria were met, the DCB was introduced into the SB with a slight protrusion into the main branch, followed by inflation for 30-60 seconds (preferably 60 seconds, unless the patient experienced angina or haemodynamic instability due to prolonged ischaemia).
Following DCB inflation in the SB, the procedure continued with stenting of the MV-MB using a new-generation DES. The sequence of deploying the DES into the MV-MB and the DCB into the SB was at the discretion of the operator.
After deploying the DES and DCB, the DES segment was subsequently postdilated using non-compliant balloons to ensure optimal stent apposition. The decision to proceed with further interventions, such as kissing balloon inflation and proximal optimisation technique (POT) together with the sequence of these and repetition, if necessary, was also left to the discretion of the operator. Procedural steps of the bifurcation PCIs (left main [LM] bifurcation and non-LM bifurcation) done with the hybrid strategy were documented. Out of the 87 bifurcation PCIs performed with the hybrid strategy, 84 PCIs were done with the DCB deployed first. Procedural steps and the sequence after DCB and DES deployment are summarised in Table 1 according to LM and non-LM bifurcation PCI.
The percutaneous coronary intervention was deemed successful if both the MB and SB achieved TIMI 3 flow, with no residual diameter stenosis exceeding 30% at the DCB segment upon final assessment.
Table 1. Procedural steps after implantation of DCB and DES in a hybrid strategy for bifurcation PCI.
| Procedural steps | Number of PCI |
|---|---|
| LM bifurcation PCI | N=30 |
| Post-dilate DES segment plus POT | 14 (46.7) |
| Post-dilate DES segment plus KBI | 8 (26.7) |
| Post-dilate DES segment plus KBI-POT | 5 (16.6) |
| Post-dilate DES segment plus POT-KBI-POT | 3 (10.0) |
| Non-LM bifurcation PCI | N=57 |
| Post-dilate DES segment only | 25 (43.9) |
| Post-dilate DES segment plus POT | 13 (22.8) |
| Post-dilate DES segment plus KBI | 11 (19.2) |
| Post-dilate DES plus KBI-POT | 8 (14.1) |
| Data are given as n (%). DCB: drug-coated balloon; DES: drug-eluting stent; KBI: kissing balloon inflation; LM: left main artery; PCI: percutaneous coronary intervention; POT: proximal optimisation technique | |
Results
A total of 401 patients with 458 lesions were included in this study, of whom 38 patients (9.5%) were lost to follow-up. The remaining 363 patients (90.5%) were included in the outcome analysis at 1 year (Figure 1).
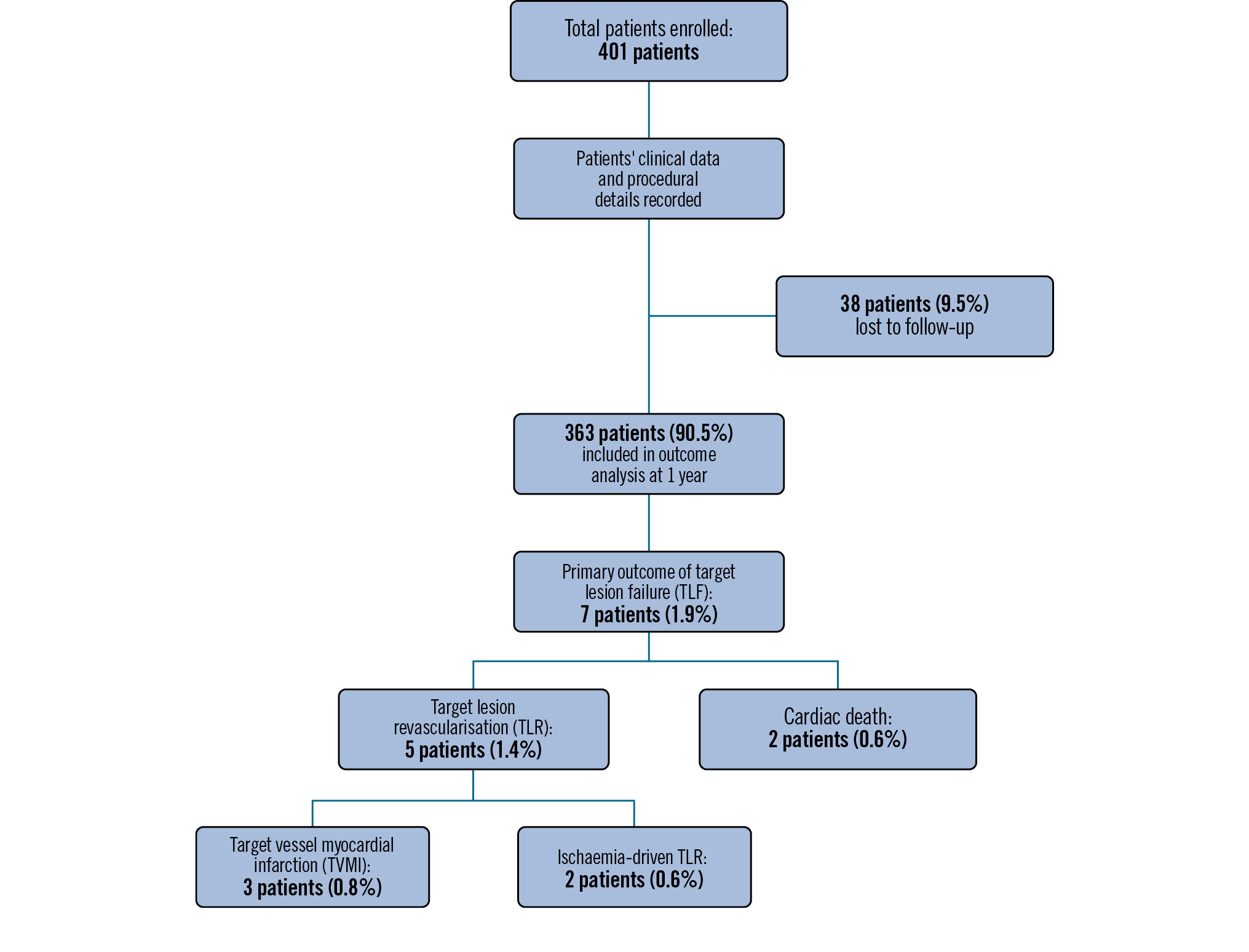
Figure 1. Study flowchart and results. A total of 401 patients were enrolled into the study. All patients’ clinical data and procedural details were recorded. In all, 38 patients (9.5%) were lost to follow-up and were excluded from the outcome analysis. A total of 363 patients (90.5%) completed the 1-year study and were included in the outcome analysis. The primary outcome of TLF occurred in 7 patients (1.9%), out of whom 5 patients (1.4%) needed TLR, and 2 patients (0.55%) died of a cardiac cause. Of the 5 patients who needed TLR, 3 patients (0.8%) had TVMI, and 2 patients (0.6%) had ischaemia-driven TLR.
Baseline characteristics
The mean age was 59.7±11.9 years, and 80.5% of the patients were male. In all, 287 patients (71.6%) were hypertensive, 243 patients (60.6%) were diabetic, 224 patients (55.4%) had dyslipidaemia, 78 patients (19.5%) had a history of myocardial infarction, and 93 patients (23.2%) had previously undergone PCI (Table 2).
Table 2. Baseline characteristics and demographics.
| Baseline characteristics | (n=401) |
|---|---|
| Age, years | 59.7±11.9 |
| Sex | |
| Male | 323 (80.5) |
| Female | 78 (19.5) |
| Ethnicity | |
| Malay | 254 (63.3) |
| Chinese | 53 (13.2) |
| Indian | 83 (20.7) |
| Other | 11 (2.6) |
| Smoking | 41 (10.2) |
| Dyslipidaemia | 224 (55.4) |
| Hypertension | 287 (71.6) |
| Diabetes | 243 (60.6) |
| History of MI | 78 (19.5) |
| History of cerebrovascular accident | 9 (2.2) |
| History of peripheral vascular disease | 3 (0.7) |
| History of chronic renal failure | 24 (6.0) |
| Previous PCI | 93 (23.2) |
| Previous CABG | 6 (1.5) |
| Data are presented as mean±standard deviation or n (%). CABG: coronary artery bypass graft; MI: myocardial infarction; PCI: percutaneous coronary intervention | |
Lesion characteristics
Most of the lesions were complex type C lesions (332 lesions [72.5%]). A total of 125 lesions (26.3%) were type B lesions, of which 100 lesions (21.8%) were B1 and 25 lesions (5.5%) were B2. Only one lesion (0.2%) was type A.
The left anterior descending artery (LAD) was the most commonly treated with the hybrid strategy, with 219 lesions (47.8%). This was followed by the right coronary artery (RCA) with 146 lesions (31.9%) and the left circumflex artery (LCx) with 57 lesions (12.4%).
A total of 35 lesions (7.6%) involved the left main stem (LMS); 33 lesions (7.3%) were LM-LAD lesions where a DES was inserted at the LM-proximal LAD segment and a DCB was used distal to the DES in the LAD, 2 lesions (0.3%) were LM-LCx lesions, and 1 (0.2%) was a saphenous vein graft-obtuse marginal artery lesion.
Overall, 87 lesions (19.0%) were bifurcation lesions, with 43 lesions (9.4%) involving LAD-diagonal bifurcations, 13 lesions (2.8%) involving LCx-obtuse marginal artery bifurcations, and 1 lesion (0.2%) involving the right posterior descending artery-posterior left ventricular artery bifurcation. Thirty lesions (6.6%) were LMS-LAD-LCx bifurcation lesions (Table 3).
Table 3. Lesion characteristics.
| Lesion characteristics | (n=458) |
|---|---|
| Coronary lesion | |
| De novo | 458 (100) |
| Lesion type | |
| A | 1 (0.2) |
| B1 | 100 (21.8) |
| B2 | 25 (5.5) |
| C | 332 (72.5) |
| Coronary artery | |
| LAD | 219 (47.8) |
| LCx | 57 (12.4) |
| RCA | 146 (31.9) |
| LMS-LAD | 33 (7.3) |
| LMS-LCx | 2 (0.4) |
| SVG-OM | 1 (0.2) |
| Bifurcation lesion | 87 (19.0) |
| LMS LMS-LAD-LCx | 30 (6.6) |
| LAD LAD-diagonal | 43 (9.4) |
| LCx LCx-OM | 13 (2.8) |
| RCA RPDA-PLV | 1 (0.2) |
| Data are presented as n (%). LAD: left anterior descending artery; LCx: left circumflex artery; LMS: left main stem; OM: obtuse marginal artery; PLV: posterior left ventricular artery; RCA: right coronary artery; RPDA: right posterior descending artery; SVG: saphenous vein graft | |
Procedure description
A total of 324 patients (80.8%) were admitted electively, while 77 patients were admitted for ACS, of whom 46 patients (11.5%) had non-ST-segment elevation myocardial infarction or unstable angina, and 31 patients (7.7%) had ST-segment elevation myocardial infarction. The radial approach was used in 345 patients (86.3%), while the femoral approach was used in 55 patients (13.7%). Intracoronary imaging-guided PCI was performed in 123 patients (30.6%): 114 patients (28.4%) with IVUS and 9 patients (2.2%) with OCT.
Atherectomy was used for heavily calcified lesions in 21 patients (5.2%), of whom 6 patients (1.5%) had rotablation, 10 patients (2.5%) had orbital atherectomy, and 5 patients (1.2%) had intracoronary lithotripsy (Table 4).
Table 4. Procedure description.
| Procedure characteristics | N=401 |
|---|---|
| PCI status | |
| Elective | 324 (80.8) |
| NSTEMI/UA | 46 (11.5) |
| STEMI | 31 (7.7) |
| Approach | |
| Radial | 345 (86.3) |
| Femoral | 55 (13.7) |
| Intracoronary imaging | 123 (30.6) |
| IVUS | 114 (28.4) |
| OCT | 9 (2.2) |
| Atherectomy | 21 (5.2) |
| Rotablation | 6 (1.5) |
| Orbital atherectomy | 10 (2.5) |
| Intracoronary lithotripsy | 5 (1.2) |
| Data are presented as n (%). IVUS: intravascular ultrasound; NSTEMI: non-ST-segment elevation myocardial infarction; OCT: optical coherence tomography; PCI: percutaneous coronary intervention; STEMI: ST-segment elevation myocardial infarction; UA: unstable angina | |
Drug-eluting stent and drug-coated balloon description
The estimated mean lesion length (DES+DCB) was 44.6±23.3 mm, with a mean DES length of 28.7±9.1 mm and a mean DCB segment length of 25.5±8.1 mm. The mean number of DES implanted per lesion was 1.3±0.6, and the mean number of DCBs per lesion was 1.1±0.3. The mean DES diameter was 3.0±0.4 mm, and the mean DCB diameter was 2.5±0.3 mm (Table 5).
The most common combination of antiproliferative drugs for the DES and DCB strategy was everolimus (DES) plus paclitaxel (DCB), in 202 (50.4%) PCIs, followed by zotarolimus (DES) plus paclitaxel (DCB) in 116 (28.9%) PCIs. Paclitaxel-eluting balloons accounted for 99% of DCBs used (Table 5).
Table 5. Description of DES & DCB.
| DES & DCB characteristics | Results |
|---|---|
| Estimated lesion length (DES+DCB), mm | 44.6±23.3 |
| Total number of DES | 1.3±0.6(1-4) |
| Total number of DCB | 1.1±0.3(1-3) |
| DCB length, mm | 25.5±8.1(12-48) |
| DCB diameter, mm | 2.5±0.3(2.0-4.0) |
| DES length, mm | 28.7±9.1(10-48) |
| DES diameter, mm | 3.0±0.4(2.0-5.0) |
| Antiproliferative drug combination ofDES and DCB | Total=401 |
| Everolimus+Paclitaxel | 202 (50.4) |
| Zotarolimus+Paclitaxel | 116 (28.9) |
| Sirolimus+Paclitaxel | 41 (10.2) |
| Biolimus+Paclitaxel | 9 (2.2) |
| (Everolimus+Zotarolimus)*+Paclitaxel | 13 (3.2) |
| (Everolimus+Sirolimus)*+Paclitaxel | 10 (2.5) |
| (Zotarolimus+Sirolimus)*+Paclitaxel | 5 (1.2) |
| (Biolimus +Sirolimus)*+Paclitaxel | 1 (0.2) |
| Everolimus+Sirolimus | 2 (0.5) |
| Sirolimus+Sirolimus | 1 (0.2) |
| Zotarolimus+Sirolimus | 1 (0.2) |
| Data are presented as mean±SD, range (min-max) or n (%). *2 DES inserted. DCB: drug-coated balloon; DES: drug-eluting stent; SD: standard deviation | |
Antiplatelet treatment
Twelve-month DAPT was prescribed in 339 patients (84.5%). Two patients (0.5%) had 1-month DAPT, 1 patient (0.2%) had 3-month DAPT, and 2 patients (0.5%) had 6-month DAPT. A total of 38 patients (9.5%) were lost to follow-up and were excluded from analysis. The reasons for a short DAPT duration were gastrointestinal bleed in 2 patients and plans for a non-cardiac operation in 3 patients.
Clinical outcomes
No TLF events happened in the hospital. All patients were discharged well, with no incidents of repeat angiography needed within 30 days. All patients were monitored and followed up for 12 months. Out of the 401 patients enrolled, 38 patients (9.5%) were lost to subsequent follow-up.
Of the 363 patients who completed the study, the primary outcome of TLF occurred in 7 patients (1.9%). Two patients (0.6%) experienced cardiac death, and 5 patients (1.4%) had target lesion revascularisation (TLR), of whom 3 patients (0.8%) had TVMI and 2 patients (0.6%) had ID-TLR (Table 6). TLF occurred at the DES segment in 3 patients and at the DCB segment in 2 patients. All patients were still on DAPT during the TLF events. The primary outcome patients’ profiles and details of the revascularisation procedure are summarised in Supplementary Table 1.
Four patients died of a non-cardiac cause at 1-year follow-up (1 patient died of haemorrhagic stroke, 2 patients died due to malignancy, 1 patient due to infection) (Figure 1, Table 6).
Table 6. Primary and secondary outcomes.
| Outcomes | N |
|---|---|
| Primary outcome (1 year) | n=363* |
| Lost to follow-up | 38 (9.5) |
| Target lesion failure | 7 (1.9) |
| Cardiac death | 2 (0.6) |
| Target vessel revascularisation | 5 (1.4) |
| Target vessel MI | 3 (0.8) |
| Ischaemia-driven target vessel revascularisation | 2 (0.6) |
| Secondary outcome (in-hospital and 30 days) | n=401 |
| Alive | 401 (100) |
| In-hospital death | 0 |
| 30-day target lesion failure | 0 |
| MACE at 1 year | |
| Cardiac death | 2 (0.6) |
| MI | 5 (1.4) |
| Stroke | 1 (0.3) |
| All-cause mortality | 6 (1.7) |
| Data are given as n (%). *Outcome analysis excluding patients lost to follow-up. MACE: major adverse cardiovascular events; MI: myocardial infarction | |
Discussion
Hybrid strategy in long diffuse lesions
The safety and efficacy of new-generation DES have been well established. However, the limitations of DES implantation, such as late and very late stent thrombosis, still remain the Achilles heel of interventional cardiology8. Stent length, overlapping stents and stent diameter are known to be consistent predictors of stent thrombosis3910. Currently, DCB treatment is the recommended treatment for ISR and received a class Ia recommendation from the European Society of Cardiology11. Multiple studies on the use of DCB in the treatment of de novo complex lesions showed promising results12. The option of a hybrid strategy combining DES and DCBs offers the advantage of avoiding a long stent length, overlapping of DES and the implantation of DES in small diameter vessels.
In our study, the estimated mean lesion length (DES+DCB) for each treated vessel was 44.6±23.3 mm. With the implementation of the hybrid strategy, the mean DES length was reduced to 28.7±9.1 mm. The remaining lesion length was complemented with a DCB, and the mean segment length of the DCB for each treated vessel was 25.5±8.1 mm. And with the use of DCBs, there were no overlapping stents.
Another strong predictor of stent thrombosis is a reference diameter of <2.6 mm10. In this study, the mean DES diameter was 3.0±0.4 mm, and the mean DCB diameter was 2.5±0.3 mm. With the use of the hybrid strategy, we were able to reduce stent implantation of stents with a small diameter <2.5 mm, thus reducing the risk of ISR and need for revascularisation.
Hybrid strategy in bifurcation disease
Coronary bifurcation lesions, which constitute about 20% of PCI procedures13, represent a unique subset of coronary artery lesions in clinical practice. True bifurcation lesions often present as complex PCI, and 2-stent strategies in these lesions are associated with higher procedural risk and complexity14. Side branch ostia seem to be particularly prone to restenosis: abnormalities in shear stress and the presence of multiple layers of struts contribute to this15.
A provisional strategy in bifurcation PCI is the first-line recommendation in most cases; however, side branch modification is commonly done during POT and kissing balloon inflation, mainly using a plain uncoated balloon, inevitably causing endothelial trauma. The notion of treating a side branch with an antiproliferative agent to prevent further stenosis in a 1-stent strategy is an attractive one. Results from BIOLUX RCT, which evaluated the feasibility of provisional stenting with DES in the MB and DCB in the SB, showed that this notion appears to be safe and effective16. This strategy resonates well with the European Bifurcation Club’s recommendation to perform the bifurcation procedure with just 1 stent17. However, this study of DCB in SB treatment was limited by low power due to the small number of patients studied18. More data are needed in terms of the technicality involved and long-term outcomes of this strategy in bifurcation PCI.
Limitations
This is a retrospective study, and we were not able to randomise patients into control and intervention arms. All enrolled subjects were from a single centre and, thus, may not represent patients from other regions.
As a national tertiary referral centre, patients returned to their local health facilities for subsequent follow-up after PCI. Thus, we were not able to track and record events or clinical outcomes of all of our patients. Subsequently, 38 patients (9.5%) were lost to follow-up.
Conclusions
The hybrid strategy of DES and DCB treatment for de novo coronary artery disease is clinically feasible and safe based on our preliminary study. Further randomised and high-powered studies are warranted to study the long-term benefits and safety outcomes of this strategy in percutaneous coronary interventions.
Impact on daily practice
The hybrid strategy of combining drug-eluting stents and drug-coated balloons in percutaneous coronary intervention presents a novel approach for treating complex coronary artery lesions. This method provides an effective solution for minimising stent length and reducing overlapping segments in long diffuse lesions and bifurcation lesions. Further data from randomised controlled trials and large-scale studies are anticipated to evaluate the long-term benefits and safety outcomes of this strategy.
Conflict of interest statement
The authors have no conflicts of interest to declare.

