Bioprosthetic aortic scallop intentional laceration to prevent iatrogenic coronary artery occlusion (BASILICA) has emerged as an indispensable procedure in patients undergoing transcatheter aortic valve implantation (TAVI) for a degenerated bioprosthetic valve. Despite successful laceration, up to 10-15% of patients suffer coronary artery occlusion requiring bailout stenting.
A 74-year-old female presented with New York Heart Association Class III symptoms on account of severe bioprosthetic valve dysfunction leading to wide-open aortic regurgitation. She had undergone placement of a 19 mm St Jude bioprosthesis (bovine; externally mounted leaflets [now Abbott]) 10 years previously. Her computed tomography images demonstrated a very high-risk anatomy for coronary artery occlusion (CAO; left main [LM] height 8 mm; length of left leaflet 15 mm; sinotubular junction 23 mm; sinus of Valsava [SoV] diameter 27 mm; and SoV height 15.2 mm) (Figure 1A–Figure 1B–Figure 1C).
Intraoperative transoesophageal echocardiography identified the posts and highlighted severe malalignment of the surgical bioprosthetic commissures relative to the native anatomy such that the ostium of the LM coronary artery was totally misaligned and very close to the post (Figure 1B, Moving image 1). Selective left cusp engagement was consequently challenging with an Amplatz left 2 guide catheter. Aortic root angiography demonstrated that while the tip of the catheter was aligned to the nadir and centre of the left cusp, the origin of the LM coronary artery was too lateral (Figure 1D, Moving image 2). The left leaflet was lacerated using the standard technique with an Astato 30gf wire (ASAHI INTECC) with electrocautery and snared into the side catheter (Moving image 3). Subsequent balloon dilation of the leaflet was performed with 5×15 mm balloon at 12 atm to widen the area which was subsequently lacerated using high energy electrocautery with a “flying V” conformation of the wire (Figure 1E, Moving image 3A–Moving image 3B–Moving image 3C, Moving image 4, Moving image 5). Given the extreme risk of CAO despite successful BASILICA, a guide catheter was inserted into the LM artery with a coronary wire in the left system and a guide extension catheter for bailout stenting. A 23 mm Evolut R valve (Medtronic) was then placed with an intentional depth of 8 mm to avoid further sinus sequestration. Following valve deployment, another Judkins left 4 guide catheter was taken through the newly deployed valve, and a selective left coronary angiography showed lacerated valve tissue invaginating the LM and impending occlusion (Figure 1F, Moving image 6). Another coronary wire was advanced down the left anterior descending artery, and intravascular ultrasound (IVUS) of the LM confirmed lacerated leaflet tissue floating in the LM coronary artery (Figure 1G, Moving image 7A, Moving image 7B). A 4×18 mm drug-eluting stent (DES) was placed orthopically from the LM into the stent of the newly deployed valve; successful placement of the DES was confirmed on IVUS imaging (Figure 1H, Moving image 8).
The success of BASILICA is predicated on the assumption that a “midline” leaflet laceration will prevent CAO only if the coronary artery is located at or near the centre of the sinus. This assumption is proportionally violated with increasing degrees of commissural malalignment, leading to greater degrees of coronary ostial eccentricity relative to the mid-cusp, and requires a change of strategy. This case highlights the unique challenges in performing BASILICA in commisurally malaligned, degenerated surgical prostheses and the persistent risk of CAO. A protection guidewire and extension catheter with careful evaluation of the jailed left sinus and LM with IVUS imaging are essential in such cases.
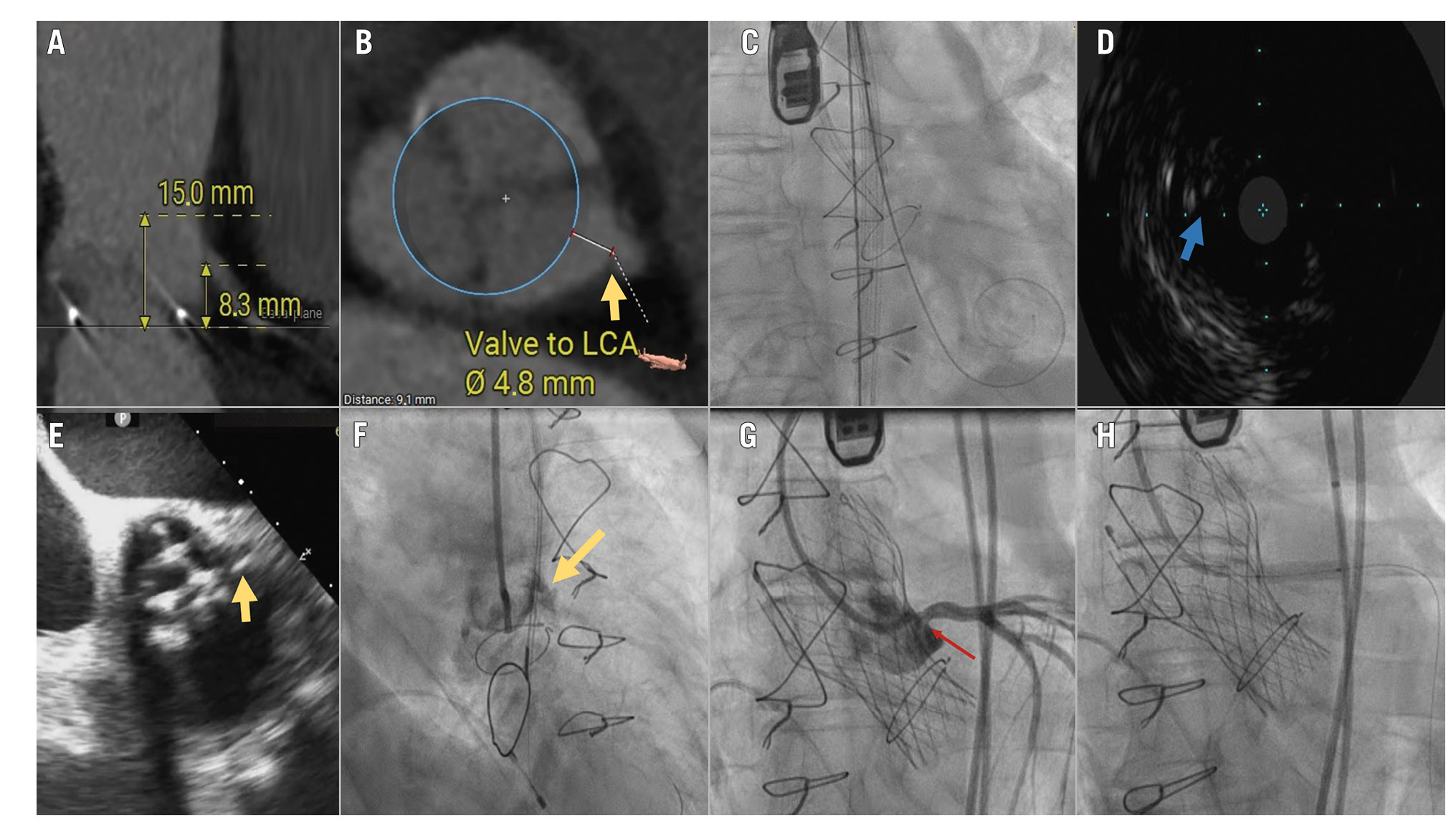
Figure 1. BASILICA and coronary protection. CT showing hostile anatomy for coronary occlusion (A,C), commissural malalignment leading to severe eccentricity of the LM coronary ostium relative to the mid-left cusp (B,C,D; arrows pointing to the LM). Following BASILICA (E), tissue prolapse of the leaflet into the LM (F,G) treated successfully with orthotopic snorkel stenting (H). BASILICA: bioprosthetic aortic scallop intentional laceration to prevent iatrogenic coronary artery occlusion; CT: computed tomography; LCA: left coronary artery; LM: left main
Conflict of interest statement
The authors have no conflicts of interest related to this manuscript to declare.

