A 75-year-old male with a history of percutaneous coronary intervention in the distal segment of the left anterior descending artery (LAD) and mid-segment of the left circumflex artery (LCx) was admitted to hospital for recurrent angina upon exertion. Initial coronary angiography (CAG) revealed severe stenosis at the LCx ostium and mild stenosis from the left main trunk (LMT) to the LAD (Figure 1A–Figure 1B–Figure 1C). Following intravascular ultrasound (IVUS) and balloon angioplasty of the LCx, he experienced chest pain, and the electrocardiogram exhibited ST-segment elevation in the precordial leads. CAG revealed Thrombolysis in Myocardial Infarction (TIMI) 2 flow in the LAD and coronary artery dissection extending from around the ostium to the proximal segment of the LAD (Figure 1D, Figure 1E, Moving image 1, Moving image 2). Upon review of the angiography performed during IVUS, a small dissection in the LAD was already evident. Therefore, iatrogenic catheter-induced coronary artery dissection, rather than balloon-induced coronary artery dissection, was considered. After passing the guidewire through the LAD, IVUS revealed a true lumen compressed by a false lumen that appeared to extend behind the calcifications, in addition to intimal dissection at the LAD ostium, but there was no obvious dissection in the LMT (Figure 1F, Figure 1G, Moving image 3). A perfusion balloon 3.0/20 mm (Ryusei [Kaneka Medix]) was inflated at the suspected dissection entry site without prolonged inflation. Consequently, angiography of the LAD, to obtain information about the dissected area, could be performed with restored LAD perfusion (Figure 1H). The perfusion balloon was also inflated with nominal pressure at the suspected distal end of the dissection to achieve fenestration (Figure 1I). IVUS revealed enlargement of the true lumen with multiple connections between the true and false lumens, followed by resolution of the chest pain and ST-segment elevation (Figure 1J, Moving image 4). CAG revealed vessel lumen expansion and coronary flow restored to TIMI 3 flow in the LAD. After dilatation with drug-coated balloons (DCBs) in the LCx and from the LMT to the LAD, CAG showed acceptable outcomes, with a residual false lumen (Figure 1K, Figure 1L). No postprocedural elevation of cardiac enzymes was observed. Follow-up CAG after 2 months showed a residual false lumen; however, healing of the dissection was confirmed after 9 months (Figure 1M).
Iatrogenic catheter-induced coronary artery dissection is rare; however, it can potentially cause life-threatening cardiac events1. Although an IVUS-guided procedure is favourable since further contrast injections may extend the dissection, performing stent implantation or creating fenestrations with cutting balloons in the precise segment is sometimes difficult to perform with only IVUS2. In our case, angiography was possible by sealing the dissection entry site with a perfusion balloon, as was restoring perfusion in the LAD. Fenestration could also be achieved with a perfusion balloon, enabling the procedure to be performed using only DCBs without crossover stenting. Perfusion balloons are primarily used for coronary perforations; moreover, their effectiveness in treating acute coronary syndrome has also been reported3. In conclusion, perfusion balloons can be a bailout option for iatrogenic catheter-induced coronary artery dissection.
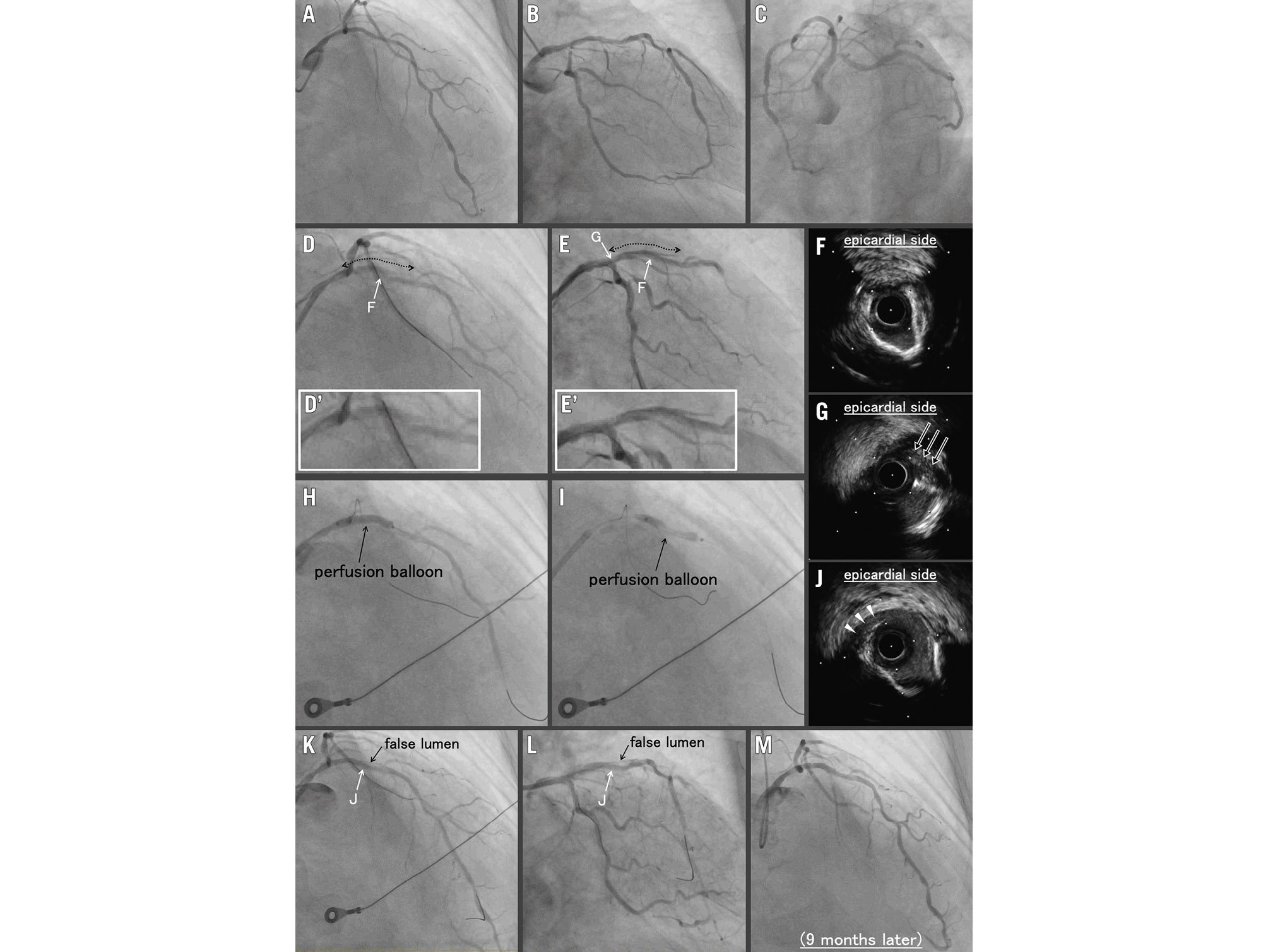
Figure 1. Coronary angiography (CAG) and intravascular ultrasound during the procedure and follow-up CAG (A-C) Initial CAG. D, E) Coronary artery dissection (dotted arrows) and Thrombolysis in Myocardial Infarction 2 flow in the left anterior descending artery (LAD). D’, E’) Enlarged images. Intravascular ultrasound (IVUS) reveals (F) a true lumen compressed by a false lumen that appears to extend behind the calcifications and (G) intimal dissection at the LAD ostium (black arrows; corresponding to white arrows in D and E). H) Angiography while sealing the suspected dissection entry with a perfusion balloon. I) Creating fenestrations with a perfusion balloon at the suspected distal end of the dissection. J – corresponding to white arrows in K and L) IVUS reveals enlargement of the true lumen with multiple connections between the true and false lumens (white triangles). K, L) Final CAG. M) Follow-up CAG after 9 months.
Conflict of interest statement
The authors have no conflicts of interest relevant to the contents of this paper to declare.

