Author: G. Sengottuvelu
A 48-year-old diabetic lady with prior percutaneous coronary intervention (PCI) to the left circumflex artery (LCX) in 2008 with a firstgeneration sirolimus-eluting stent had an episode of definite very late stent thrombosis (VLST) in 2012. PCI was carried out with a balloon angioplasty (BA) and she was maintained on prasugrel and aspirin.
Within weeks after changing prasugrel to clopidogrel after 18 months of BA, she again presented with VLST in 2014. A coronary angiogram showed occlusion of the LCX stent (Figure 1A, Moving image 1). After thrombus aspiration, optical coherence tomography (OCT) imaging (Figure 1B-Figure 1F) showed thrombus within the stent (no uncovered struts) and areas of high attenuation within the neointima, suggesting neoatherosclerosis (Figure 1C, #).
Intravascular ultrasound (IVUS) imaging (Figure 1G-Figure 1K, Moving image 2, Moving image 3) showed areas of positive remodelling of the vessel wall outside the stent with aneurysmal dilatation causing late acquired stent malapposition which was the obvious cause for recurrent VLST.
Neoatheroma seen by OCT is possibly an innocent bystander as shown by thick intima with superimposed thrombus. High-pressure non-compliant balloon post-dilation followed by re-stenting with a bare metal stent was carried out and she was continued on aspirin and prasugrel (Figure 1L, Moving image 4).
Late acquired malapposition seen by IVUS is the cause of VLST, and neoatherosclerosis seen on OCT is possibly an innocent bystander. OCT with high resolution is excellent for intraluminal evaluation, such as for uncovered struts and neoatherosclerosis, whereas IVUS with good penetration is better for imaging beyond the stent and vessel wall such as in the case of positive remodelling. Thrombus obscures optimal OCT imaging, whereas IVUS is poor for assessment of strut coverage or neoatherosclerosis. The use of a single imaging modality would have missed the diagnosis in this case where multimodality imaging was crucial to get a complete diagnosis.
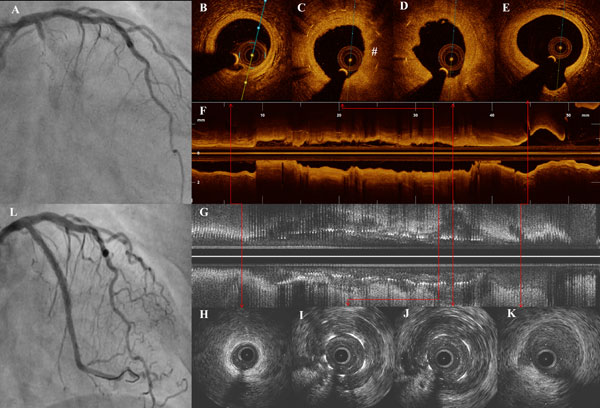
Figure 1. Multimodality imaging of recurrent VLST. Angiogram with longitudinal and axial images of IVUS and OCT. A) Initial angiogram showing total occlusion of the stent in proximal LCX. B) OCT image distal to stent. C) & D) OCT images across a stented segment corresponding to areas of positive remodelling on IVUS showing thrombus and neoatherosclerosis (#). E) Vessel proximal to stent. F) Longitudinal OCT reconstruction of the stented segment. G) Longitudinal IVUS image showing areas of acquired late malapposition. H) – K) IVUS sections corresponding to B to E showing covered struts and positive remodelling of the vessel. L) Final result after PCI.
Supplementary data
[/custom_font]
Moving image 1. VLST with total occlusion of the stent in the prox-imal LCX.
Moving image 2. Longitudinal (reconstructed) and axial (acquired) IVUS runs showing the malapposition.
Moving image 3. Longitudinal (reconstructed) and axial (acquired) IVUS runs showing the malapposition.
Moving image 4. Final result after PCI.
